Fundraising with Heart: The Baby Blue Sound Collective
Last month, Sisters by Heart was honored to attend Baby Blue Sound Collective's performance in Miami, FL. The Baby Blue Sound Collective is a musical ensemble composed of pediatric heart surgeons, cardiologists, nurses, and other CHD care providers from around the country. The BBSC currently performs at many of the pediatric cardiology and cardiac surgery medical conferences throughout the USA and Europe: the personnel of the band is different for each performance, and primarily depends upon who is on the course faculty at the particular meeting. The songs and genres vary, but include classical, jazz, pop, musical theater, blues and rock.
We were blown away by the talent of this incredible group of clinicians! The BBSC encouraged those in attendance to make donations throughout the night - and through their generosity, Sisters by Heart raised over $600! We are so grateful to Dr. Gil Wernovsky and the entire BBSC crew for their continued dedication in supporting CHD families.
Sharing HOPE: An exciting opportunity
Hello Sisters by Heart Family! SBH is invited to participate in a hugely impactful project with Empowered By Kids.
Sisters by Heart was founded from a deep desire to spread Hope to newly diagnosed families. How would you have reacted to a "Book of Hope" containing stories of children and families living with an HLHS diagnosis at the time of your diagnosis? Sisters by Heart feels strongly that sharing your hope and inspiration with families who are walking our journey can be a soul-shifting event for the newly diagnosed. The "Book of Hope" will be provided in Sisters by Heart care packages and given to care centers across the country at no cost for distribution to newly diagnosed families.
We'd love to capture a few dozen incredible stories to include in the HLHS "Book of Hope." To participate, please prepare a write up (250 word maximum) outlining your journey with HLHS. Your story should reflect words of inspiration that you needed at diagnosis - reflecting that it is indeed not fair, but you will get through this and there are brighter days ahead. You can also supply a photo or artwork for the book.
No demographic data will be revealed in the Book of Hope. Your story will include you/your child's first name or patient name (for teen/adults). Patient ages will be included.
Empowered by Kids has worked with two other pediatric rare disease communities to create their Books of Hope, which can be viewed here:
Interstage Care and Mortality (surgical v. non-surgical sites)
Special thanks to Dr. David Schidlow
The journal, Pediatric Cardiology, published a study in August, 2014: Site of Interstage Care, Resource Utilization, and Interstage Mortality: A Report from the NPC-QIC Registry. This study was completed utilizing data from the National Pediatric Cardiology Quality Improvement Collaborative patient database.
The abstract can be found at the following link: http://www.ncbi.nlm.nih.gov/pubmed/25107545
What is the background of this study?
o Medical problems and early death remain a problem for children with hypoplastic left heart syndrome (HLHS) during the outpatient “interstage” period between the first (Norwood) and second (Glenn) operations.
o The National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) identifies differences in the care of interstage patients in the hopes of learning the best way to care for these children during this sensitive time.
o One difference in care is the place where children receive interstage care. Some are cared for at the surgical site (SS) that performed the Norwood operation. Others are cared for at a non-surgical site (NSS), which could mean a hospital that does not perform the Norwood operation or a private cardiologist. Among those who are followed at a NSS, the distance to the surgical site can vary greatly.
The aims of this study were to answer the following questions:
o Where do HLHS patients receive their interstage care? The surgical site (SS) that performed the Norwood operation, a non-surgical site (NSS), or at a combination?
o How far is the NSS from the SS for those children who are followed at a NSS or at a combination of sites?
o Are there differences in the number of medical problems or deaths associated with the site of interstage care and/or the distance from the surgical center?
How was this study performed?
o The researchers looked back at patients with HLHS entered into the NPC-QIC database over an approximately five-year period (July 2008 to February 2013). The site of each patient’s interstage care was noted as (1) the SS that performed the Norwood procedure, (2) a NSS as described above, or (3) a combination. The distance from the SS to NSS was identified for patients in categories 2 and 3. The number of interstage medical problems, emergency department (ED) visits, readmissions to the hospital, and deaths were identified for each of the three groups.
What were the results of the research?
o Most patients (60%) received their interstage care at the SS. The remaining patients received their care at a NSS (17%) or at a combination of sites (21%).
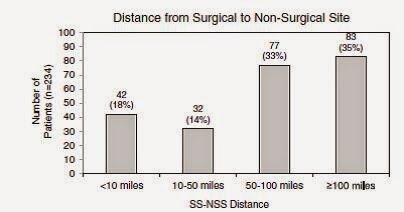
o The patients who received interstage care at a NSS or at a combination of sites were followed at a variety of distances. A large number (68%) of those patients were followed at a distance of 50 miles or greater from the surgical site. The following figures are taken directly from the paper.
o Patients followed at the SS were more likely to have emergency room visits and readmissions. Conversely, patients followed at a NSS or at a combination of sites were more likely to have problems identified with breathing and/or feeding.
o Despite these differences, there were no differences in the rates of death or in the reasons for death among the three groups. Similarly, there was no difference in rates of death based on the SS-to-NSS distance.
o There were 66 patients, approximately 10% of the entire group, who unfortunately did not survive the interstage. It was notable that among those 66 patients, 37 (55%) percent of them died in their home or in an emergency department.
What are the limitations to this study:
o There were several limitations to this study. The main limitations related to the level of detail that was able to be ascertained about these patients.
o The NSS and combination categories were very broad. As noted above, they could be anything ranging from a large medical center that simply does not perform Norwood operations to the office of a single practitioner far from a medical center. This study could not distinguish smaller differences between the two.
o The significance of more breathing and feeding problems identified at the NSS or combination is unclear. It is not known if these patients truly had more problems, or if the fact that these problems were identified reflected more vigilance on the part of the caregivers. Another limitation is that these categories are very broad. Feeding and breathing problems could mean different things to different caregivers. This lack of detail makes a refined analysis somewhat difficult.
What are the takeaway messages considering the results and limitations of this study?
o The site of interstage care does not seem to affect the likelihood of a patient passing away during the interstage period. Similarly, the distance of interstage care from the SS that performed the Norwood does not seem to affect the rate of death.
o More ED visits and readmissions occurred in the SS group, and conversely, more feeding and breathing problems were identified in the NSS and combination groups. As noted above, these differences did not seem to have an effect on death.
o Finally, the mortality rate still remains high at approximately 10%, with many patients dying at home or in an emergency department. This is an important reminder that we still have room to improve interstage care and decrease mortality.
If you missed the first three installments of Research Explained, you can link to them here: https://www.jcchdqi.org/research
Sano vs. BT Shunt
Popularity of the National Pediatric Cardiology Quality Improvement Collaborative's (NPC-QIC) Research Explained is growing. The third installment, brought to you by NPC-QIC's Research Committee, analyzed differences in the Sano and BT shunt used during the Norwood procedure - "Comparison of Shunt Types in the Norwood Procedure for Single-Ventricle Lesions", published in The New England Journal of Medicine in May 2010.
Our families often discuss this same subject, "Sano vs. BT" and are looking forward to your comments regarding this comparison.
Main Finding from this Study
While there has been great improvement in care for patients with hypoplastic left heart syndrome and other similar single ventricle lesions that require the Norwood procedure, these patients are still at great risk. When the Norwood procedure is performed there are 2 different ways blood can be supplied to the lungs. A right ventricular-to-pulmonary artery shunt (RVPAS) is placed directly from the right side of the heart to the pulmonary arteries by making a cut in the heart muscle. A modified Blalock-Taussig shunt (MBTS) is placed from an artery that supplies the head and arm to the pulmonary arteries. Each shunt has advantages and disadvantages. The MBTS may cause less blood to flow to the heart muscle through the coronary arteries, but the RVPAS may not allow the pulmonary arteries to grow well and makes a scar on the muscle of the heart. It was not known if one of these shunts were better than the other.
This study describes a comparison of two groups who were randomly assigned to get one shunt type or the other at the time of their Norwood surgery. The authors of this study concluded that in infants undergoing the Norwood procedure, survival without requiring a heart transplant was better at 1 year of age in those receiving a RVPAS than those receiving a MBTS.
About this study
Why is this study important?
This was a very important study because doctors at many different medical centers worked together to find answers to questions that could not be answered by one medical center alone. This is the first time that this type of study was successfully performed in congenital heart surgery, and has helped usher in a new era of cooperation between centers in doing research to improve outcomes in these patients. The number of patients at any single center would not be large enough to be certain that difference are not just based on random events or differences between individual patients, but rather based on an effect of one particular intervention or another. Statistical calculations may be used to correct for individual differences, but can only be used when the groups of patients studied are large. Many other studies have come from the information collected in this study because so many different medical centers worked together to contribute information. This study was also the first fair comparison between shunt types because patients were randomly assigned to a type of shunt. This means that in such a large group, any difference seen between those with the two types of shunts is most likely due to the type of shunt.
In addition, this is a very large group of patients with this heart defect about whom we have a lot of very good baseline information. It will be very valuable to continue to follow them over time, even for their entire lives.
How was this study performed?
This study enrolled patients from 2005-2008 who required the Norwood procedure at 15 medical centers in the United States and Canada. The patients were randomly assigned to one shunt type when they had their Norwood surgery. They were followed after surgery for 12 to 52 months depending on when they entered the study. The main comparison was how many from each group survived to 1 year of age without needing a heart transplant. In addition, they compared how many catheterization procedures each group underwent and the function of the hearts by echocardiogram (echo) for each group.
What were the results of the research?
o 275 patients with MBTS were compared to 274 patients with RVPAS.
o At 1 year of age the RVPAS had more patients alive without needing a heart transplant (74%) than the MBTS group (64%).
When they followed the patients they could for longer than 1 year the difference between the groups disappeared.
At centers that did a lot of Norwood procedures every year there was no difference between shunt types even at 1 year.
o The group getting the RVPAS underwent more catheterization procedures than the MBTS group, mostly to perform interventions to increase the size of the pulmonary arteries.
o At the end of the study there was no difference between shunt groups in the function of their heart by echo.
What are the limitations of this study?
This study went on for many years and patients were enrolled at different times so they were followed for different lengths of time. The main comparisons between groups were made when all patients were about 1 year old. This may not be long enough to know which shunt type is better. Differences at 3 years were also examined and published recently1. These data confirm that differences seen at 1 year did not continue. The number of patients alive without heart transplant was very similar between the two groups (67% for RVPAS vs. 61% for MBTS), even though cardiac function by echo was a little better in the MBTS group and those in the RVPAS group underwent more catheter procedures. A further extension of this trial is ongoing to see what happens at 6 years old.
Differences in many features of patients might be studied, but deciding which are important (other than survival without heart transplant) is difficult. As well, many differences in how patients are treated at different centers can be seen. But since the patients were randomly sorted into groups for comparison based only on the type of shunt they received and not other aspects of care (such as using a certain medication), conclusions about other aspects of care would be very difficult.
What are the takeaway messages considering the results and limitations of this study?
For the 1st year of life, survival without heart transplant is better in those who get a Norwood with RVPAS than those who get a MBTS. After that, there is not a clear advantage to have one shunt over another, but as they continue to collect more information over time, new knowledge may be gained. The group that had RVPAS had smaller pulmonary arteries and underwent more catheterization interventions to try to improve the size of their pulmonary arteries.
1 Newburger JW, Sleeper LA, Frommelt PC, Pearson GD, Mahle WT, Chen S, Dunbar-Masterson C, Mital S, Williams IA, Ghanayem NS, Goldberg CS, Jacobs JP, Krawczeski CD, Lewis AB, Pasquali SK, Pizarro C, Gruber PJ, Atz AM, Khaikin S, Gaynor JW, Ohye RG; Pediatric Heart Network Investigators. Transplantation-free survival and interventions at 3 years in the single ventricle reconstruction trial. Circulation. 2014 May 20;129(20):2013-20.
Many thanks to NPC's Research Committee for continuing to assist parents in understanding research studies that relate to our children with HLHS.
NPC-QIC Research and Publications Committee 2014-2016
Jeff Anderson, Chair, Cincinnati Children's Hospital Medical Center
Jean Ballweg, Le Bonheur Children's Hospital
Katie Bates, Children's Hospital of Philadelphia
Michael Bingler, Children's Mercy Hospitals and Clinics-Kansas City
Clifford Cua, Nationwide Children's Hospital
Nancy Halnon, Mattel Children's Hospital UCLA
Garick Hill, Children's Hospital Wisconsin
Colleen Melchiorre, Parent
Patrick O'Leary, Mayo Clinic
Sarah Ortiz, Parent
Matt Oster, Children's Healthcare of Atlanta
David Schidlow, Boston Children's Hospital
Julie Slicker, Children's Hospital Wisconsin
Karen Uzark, University of Michigan Congenital Heart Center
NPC-QIC 2014 Fall Learning Session!
Registration for the NPC-QIC 2014 Fall Learning Session is now open! Sisters by Heart and NPC-QIC want to send YOU to the Fall Learning Session November 7-8, 2014! Together, Sisters by Heart and NPC-QIC are offering parent travel scholarships, valued at $500 each, to three parents to attend the learning session in Cincinnati, OH. If you are new to the HLHS world, haven’t heard of NPC-QIC before, or have questions about what NPC-QIC does, we have put together a little information for you. The National Pediatric Cardiology Quality Improvement Collaborative’s mission is to improve the care and outcomes for children with cardiovascular disease. NPC-QIC’s current quality improvement project is working to improve survival and quality of life for infants with Hypoplastic left heart syndrome (HLHS) during the "interstage" period between discharge from their initial open heart surgery- Stage 1 Norwood - and admission for a Stage 2 biredirectional Glenn procedure. Fifty-five (55) centers from across the country have come together with parents to improve the care for HLHS babies.
Ask any parent who has attended a NPC-QIC learning session about their experience and their reaction will be the same; it is life changing. Natasha Sawyer, Sisters by Heart board member, shared her experience on her personal blog after attending her first learning session in January of 2013:
“The conference was more than I could have ever imagined it would be. I'm not sure what I expected, but it definitely wasn't this. Teams consisting of cardiologists, nurse practitioners, nurses, dieticians, therapists, social workers, and parents filled a large conference room and the excitement began. Over 100 people were in attendance, including 15 parents, representing centers from across the country. From the moment I walked in, I felt welcomed. I felt important. Doctors and team members expressed how thrilled they were to see so many parents in attendance and how crucial we are to the success of the collaborative.
Before the conference, I did not fully comprehend how amazing pediatric cardiologists and their team members are. Sure, I knew it took a special kind of person to work with babies and children with life-threatening heart defects, but until this weekend, I did not see it as more than just their "job". Please bare with me for a few minutes, I am still on an "emotional high" from the past two days and I am desperately trying not to jump up and down and shout for joy while I try my best to describe what I witnessed.. The members of the NPC-QIC have more passion for saving Hypoplastic Left Heart Syndrome babies than you can even begin to imagine. They are not satisfied with their current programs. They are not satisfied with the percentage of babies surviving from the first to second surgery, even though just 30 years ago these babies were being sent home to die. They are spending so much time and energy going above and beyond what is expected of them to change the future of children born like my son. They are changing the quality of life for these kids- kids and families they have yet to meet and have no tie to! I used to think Cardiologists were keeping their ideas to themselves, not wanting to share their "trade secrets" with anyone else. This weekend, I saw how open every team was to sharing their "secrets" with their colleagues. I watched cardiologists and team members from different centers take notes as another shared what is working for their center.
This weekend, I saw not only passion for caring for HLHS kids, but a fire to continue to make advancements and improvements for these children. I am so humbled by this experience, and feel forever indebted to these physicians and care team members who are helping our children continue to defy the odds. I cannot wait to share everything I have learned with my team's collaborative coordinator.” Natasha Sawyer, HLHS Mom, http://www.ramblingsofaheartmomma.blogspot.com/2013/01/npc-qic-2013-wint...
Parents with a single ventricle child, who required a Norwood or Norwood varient surgery may attend the learning session and/or apply for a travel scholarship. You do not need to be currently involved with your child's interstage clinic.
Sisters by Heart will be accepting travel scholarship entries until September 1, 2014. In order to be considered, please send an email with "Learning Session Scholarship" in the subject field to info@sistersbyheart.org with the following information:
Name
Address
HLHS child's name and DOB
HLHS child's hospital
A brief paragraph on why you would like to attend
If you are interested in attending and can make arrangements for childcare/time off work, please apply! This is such a wonderful opportunity to share your opinions, answer questions from a “professional” perspective as a parent, and most importantly be involved in helping to improve care for HLHS children.
Awarded scholarships will be announced via email by September 8, 2014.
Please make sure to register for the event using the following link if you will be attending the Fall Learning Session! http://events.r20.constantcontact.com/register/event?oeidk=a07e9kkxcx922...
We look forward to seeing you in Cincinnati in November!
Can the Left Ventricle Be Taught to Grow?
We're excited to share with the HLHS community, a second installment of "Research Explained" courtesy of the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC). NPC-QIC's Research and Publication Committee reviewed a study published in November of 2012 - a subject we've covered previously - on Boston Children's Staged Left Ventricular Recruitment (SLVR) for borderline HLHS patients.
We know many of you are interested in reading more about the SLVR program, and some of our Sisters by Heart families have and are currently undergoing SLVR in Boston.
Special thanks to Colleen Melchiorre (Mom to Paul, HLHS) and Dr. David Schidlow for their dedication in bringing us the following "Research Explained."
The Journal of the American College of Cardiology published a study in November 2012: “Staged Left Ventricular Recruitment after Single-Ventricle Palliation in Patients with Borderline Left Heart Hypoplasia.”
The abstract can be found at the following link: http://www.ncbi.nlm.nih.gov/pubmed/23062531
The NPC-QIC Research and Publication Committee reviewed this article, and a summary of the findings can be found below.
Main Finding from this Study:
Most children with hypoplastic left heart syndrome (HLHS) require three surgeries in the beginning of their lives for survival: the Norwood, Glenn and Fontan surgeries. This result of these surgeries is a heart that only has one pumping chamber (instead of the usual two chambers). For children with HLHS, the right ventricle pumps blood to the body. The process of these surgeries all together is called “single-ventricle palliation”, or SVP. (SVP is the term used in the article, but it might be more familiar to many readers as the “Fontan route”.)
SVP is recommended for most children with HLHS. This is because the left ventricle is too small to help pump blood to the body. In some children, however, the left ventricle is “borderline”, meaning that it might, with the help of multiple surgeries and other procedures designed to promote growth, be able to do the work of pumping blood to the body.
The authors of this paper describe an approach at Boston Children’s Hospital for children with borderline hearts. They show that for certain patients, it is possible to get the left ventricle to grow using a combination of different surgeries and other procedures. Some of the patients who undergo these surgeries and procedures are able to have a “biventricular” circulation, meaning the left ventricle pumps blood only to the body and the right ventricle pumps blood only to the lungs. This is more similar to a healthy normal heart. Perhaps more importantly, this demonstrates that there is the potential for growth of the left ventricle in patients with borderline left heart structures.
About this study:
Why is this study important?
Many children with HLHS who undergo SVP do well. Unfortunately, however, many babies and children do not survive SVP and others have medical problems related to the heart and other organs. This has prompted investigators to explore the possibility of getting the left ventricle to grow in the hope of keeping the left ventricle as the chamber that pumps to the body (this is called a biventricular circulation). These children could (we don’t know yet) have better survival and fewer medical problems than those that undergo SVP.
The authors of this paper describe ways of getting the left ventricle to grow; they call this “staged left-ventricular recruitment”, or SLVR. SLVR procedures include surgeries and catheter-based procedures designed to promote blood flow through the left side of the heart. This includes procedures on the mitral valve, the aortic valve, and within the left ventricle itself. These are all components of the heart that are affected by HLHS, and patients must meet certain qualifications of these components to be a candidate for SLVR.
How was this study performed?
The researchers looked back at patients diagnosed with borderline heart at Boston Children’s Hospital between 1995 and 2010. They compared 34 patients with borderline hearts who underwent traditional SVP, and 34 patients who underwent SLVR. They compared the sizes of different left-sided heart structures. Specifically, they compared the size of the mitral valve, aortic valve, and left ventricle.
What were the results of the research?
At birth, the sizes of the left heart structures were similar in both groups of patients, although the patients in the SLVR group tended to have a slightly larger left ventricle, and patients in the SLVR group were more likely to have had a procedure as a fetus (during the pregnancy) or shortly after birth to open a blocked aortic valve.
Patients in the SLVR group did demonstrate growth in their left-sided heart structures. Specifically, they had a larger mitral valve, aortic valve, and left ventricle than patients who had SVP. The most growth was seen after the Glenn surgery.
12 of the 34 patients in the SLVR group were able to achieve biventricular circulation. 18 of the patients had either Glenn or Fontan type hearts, and 1 underwent transplant. Those with Glenn or Fontan circluation will either continue with SLVR or undergo SVP.
Patients who had a traditional SVP typically had 3 surgeries, whereas patients who underwent SLVR typically had 4 surgeries.
Patients who had a small hole created in the top heart chambers to direct blood flow into the left ventricle were more likely to have growth of left-sided heart structures.
There were 3 deaths (8%) in the SLVR group and 7 deaths (20%) in the SVP group. Although this difference was noted, the number of patients in the study overall was too small to know if that difference was due to the way they were treated.
What are the limitations of this study?
The study looked at a small number of patients. This limits the ability to draw conclusions that can be applied to the general population. Borderline patients encompass a wide range of patients with many different sizes of the left side of the heart.
There may be aspects of the hearts in the SLVR that are different from the SVP group. Patients in the SLVR group were more likely to have a procedure as a fetus or newborn to relieve blockage of the aortic valve. This may mean that there are differences between the two groups despite the size of their left hearts being similar.
This study does not describe how the SVP and SLVR patients are doing clinically, either in the short or long term.
Important questions that could be addressed in the future include
What does the future hold for promoting the left side of the heart to grow?
How are the SLVR patients doing clinically, and what are their long-term outcomes? How do they compare to the SVP patients?
When is the best time to undergo SLVR?
What are the takeaway messages considering the results and limitations of this study?
This study shows promise for promoting growth of the left ventricle in patients with borderline heart. Future study is required to explore the best way to achieve that growth, but this study offers hope.
In order to undergo SLVR, children must meet certain qualifications. It is important to relaize that SVP is recommended for most children with HLHS. In a select group of patients with HLHS - those with a borderlne heart - surgeries and other procedures to encourage the left heart structures to grow are possible. Among such patients, some but not all, will achieve a biventricular circulation.
SLVR includes a variety of surgeries and catheter-based procedures on different parts of the left heart (the mitral valve, aortic valve, and ventricle), and most patients who undergo SLVR will have a Norwood and Glenn procedure prior to achieving a biventricular circulation.
Compared with patients who undergo SVP, patients who undergo SLVR have larger left heart structures, and 12 out of 34 patients who underwent SLVR were able to achieve a biventricular circulation.
More studies are required to understand the best way to promote left heart growth and to understand the short and long-term quality of life for patients with biventricular circulation.
The Bottom Line:
Doctors at Boston Children's Hospital are working to grow the left side of the heart for some children with HLHS. These procedures are still being studied, but they seem to help the left heart grow for some children. In order for your child to qualify, he or she must meet certain criteria. You may wish to talk to your cardiologist about SLVR, and whether your child may be right for it. Dr. Emani (the author of the article reviewed here) can also be contacted at sitaram.emani@cardio.chboston.org.
Using Crisis to Create: The Asher James Foundation
In June, Sisters by Heart President, Stacey Lihn, presented at the Mended Little Hearts' National CHD Symposium. Following, she was able to meet and talk with HLHS parents across the country. Jen DeBouver is one of many parents that inspired Stacey, and we've asked Jen to share her journey and advocacy efforts - to educate parents on the risks of blood clots in our CHD community and how you might be able to help.
When I was pregnant with my son, my second child, I thought nothing could go wrong – not this time. I had just lost my daughter Olivia at 27 weeks. She no longer had a heartbeat the doctor told us. When it came around 26 weeks of pregnancy with Asher, I was a nervous wreck. My husband and I were at a 26 week check-up when the ultrasound tech left to get the doctor. I couldn’t believe something was happening again around the same time as Olivia. When the doctor returned, he told us that he wanted us to get a second opinion on Asher’s heart because he saw something but wanted to make sure.
We had an echo done and found out that Asher had Aortic Stenosis. The doctor gave us two options – wait until he was born in which his heart defect would develop into HLHS or have a fetal intervention. As a parent we wanted to do the best possible thing for our baby so we decided to do the fetal intervention. A week later we flew from Chicago to Houston to have the fetal intervention.
When we got to Texas Children’s, it was a full day of testing to see if we were a candidate for the fetal intervention. This is when we learned that in a week, Asher’s heart had gotten worse. He had developed coarctation of the arch and had leaks in his mitral and tricuspid valve. The cardiologist started crying and told us that our baby had no idea that he was sick. We met with the entire team and one of the doctors told us that without the fetal intervention, Asher wouldn’t make it to birth and that it was a Hail Mary that he would make it through the procedure. Asher was born on September 10, 2012, at 36 weeks – 9 weeks after the fetal intervention. After we had a very successful fetal intervention, we started calling Asher our little Fighter. Hours after being born, he had to have a cath procedure to re-inflate the balloon that was inserted during the fetal intervention. At 11 days old, he underwent his first surgery to fix his aortic arch.
Asher rocked every procedure and was doing amazing. But at 4 weeks old all that changed. One day Asher looked amazing and then the next he started looking red and puffy and continued getting puffier from there. After 2 days of being swollen, we found out that blood clots had developed in his jugular veins and arms, restricting blood flow from his head to his heart. The hematologist tried different medications on him, some seemed to work and some didn’t. She told us that they were using scaled down adult medications because there aren’t any medications designed for children. She also told us that there weren’t any foundations supporting blood clots in children.
Asher lived for 6 weeks before he lost his battle to these blood clots on October 23, 2012. After everything that his hematologist told us, I knew that I wanted to continue Asher’s fight by starting a foundation in his memory for children’s blood clots. So a few months later, my husband and I started the Asher James Congenital Heart Disease & Thrombosis Foundation. We wanted to let others know that their children were at risk for clots when hospitalized because we had no idea this could happen until it happened to us.
This year we held our first Children’s Blood Clot Awareness Day at Ann & Robert H. Lurie Children’s Hospital of Chicago to inform families and staff of blood clot awareness. We spoke on Capitol Hill to both Congress and the Senate on children’s blood clots and shared Asher’s story.
In the Fall, we are holding our first blood clot awareness walk. We know that Asher is still with us and is making a difference in children’s lives and we continue his fight through awareness, and one day, research in children’s blood clots. Find out more about our foundation at www.asherjamesfoundation.org.
Thank you, Jennifer, for sharing Asher's story and your courageous fight to raise awareness and answers for both the CHD community and all children at risk for thrombosis. Feel free to "like" the Asher James Foundation on Facebook at https://www.facebook.com/asherjamesfoundation and show Jen your support by commenting on the Foundation's page and/or sharing your story about how thrombosis/blood clots affected your CHD journey.
CHD Kids and School Special Services
Summer is almost over and many HLHS children are headed to school - for the first time or as returning students. Trent Hamilton, HLHS dad and Middle School Principal, generously shared his wealth of information with Sisters by Heart on educational benefits and services for CHD children in the public school system. Thank you, Trent, for sharing this information with our families!
Several people in our CHD support group have recently had questions about getting special services for the kids who are starting school this year. Specifically, we have been discussing the differences between Special Education services through the Individuals with Disabilities Education Act (IDEA) and Section 504 of the Rehabilitation Act of 1973 (Section 504), and which would be appropriate for their CHD child. As a school principal, I deal with both Section 504 and IDEA students on a daily basis. I hope that the following blog will help you make the right decisions to provide assistance and protection to your CHD child as they start the new school year.
Basically, the two laws are similar in that they both provide educational benefits to kids with disabilities, but they differ in their eligibility requirements and the types of benefits that are provided. The requirements for eligibility under IDEA are stricter than those under Section 504, but IDEA provides more benefits than does Section 504. Essentially, all students under IDEA are also protected under Section 504, but not all students under Section 504 are protected by IDEA. It is easier to place a student under Section 504 because it has less procedural criteria, but these students are generally provided less assistance and monitoring by the school. IDEA status is more difficult to get because there are more specific criteria and it has much stricter regulation, but it does provide more types and degrees of assistance and special services to the student. Section 504 protects people for their lifespan in many areas, including school, employment, and transportation, while IDEA only addresses the special education of students from ages 3 to 21.
Students are eligible for IDEA if they have a specific impairment or condition that adversely affects their educational performance. These impairments/conditions can include, but are not limited to: autism, learning disabilities, speech/hearing impairments, emotional disturbance, or other health impairments, but the condition MUST adversely affect their education. Students are eligible for Section 504 if they have a condition that substantially limits a major life activity, even if the condition does not affect their education. Major life activities include: walking, seeing, speaking, breathing, learning, and working. But Section 504 conditions do NOT have to have an educational affect.
IDEA requires that students be placed in the most appropriate learning environment for them individually. This can include regular or special education classes. It also requires that each student has an individualized education program (IEP), which provides specific modifications and accommodations to help the student succeed academically. Section 504 generally places students in a setting that is comparable to that of students who are not disabled. It also provides some accommodations, but these are usually used in the regular educational setting.
So, which type of services is right for your child? This depends on the level that your child’s CHD has affected them and their development. If your child’s CHD caused them to have any type of developmental or learning disability, then IDEA is probably the right program. If your child’s CHD slows them down physically, but has not affected their learning or development, then Section 504 is probably best. There are obviously exceptions to these, so be sure to consult your child’s school if you aren’t sure which is right for you.
You might be wondering why you need any type of service at all if your child doesn’t have any learning or developmental issues. As a principal and a CHD parent, I highly recommend that you pursue some sort of protection for your child at school. While your child may not need accommodations or special services in order to succeed academically, they may need some of the other protections that are provided under Section 504. One of these protections involves attendance. Many states require that students attend 90% of the available school days and, even if an absence is for approved medical reasons, a student can be retained for excessive absences. If a student has protection under Section 504, special accommodations can be made in the event of an extended illness or hospitalization. Also, your child may not experience severe educational deficits early in their school years, but if they do later in life, having a 504 plan can make it easier to get accommodations or even move to IDEA protection. Section 504 also makes it easier to get certain exemptions from activities, like running, lifting weights, etc. In addition to all of this, the Section 504 plan follows your child through school as a record and every new teacher is required to review it during the school year. This means that each new teacher will be notified of your child’s condition and know what your child needs.
I hope that this information helps you in making the right educational decisions for your CHD child. If you still have questions, I encourage you to speak to your school’s counselor or special education diagnostician. Again, your CHD child does not have to have either one of these services, but I assure you that my son (HLHS) will, at least, have a Section 504 plan.
Trent Hamilton
Heart Dad & Middle School Principal
HLHS Collaborative: June's Action Period Call
The Action Period call started as usual, with the typical data review. For those who have allowed your center to share data with the Collaborative, it is collected for research and quality improvement. To date there are 1304 patients in the registry. Despite the typical data review, the focus was on the mortality rate because decreasing mortality is one of the primary goals. Prior to the inception of the Collaborative in 2008, interstage mortality rates in the medical literature were around 10-15%. The NPCQIC mortality rate at times seemed to hover around 10%. However, when looking at all the data, it shows that the mortality from 2008 to 2014 is 8.1%. Then came the big news, when looking at a more recent period, from January 2013 to May 2014 the Collaborative interstage mortality rate was 6%! This was the first time that the Collaborative was able to statistically show a reduction in mortality. The thought is that by working together, the involved centers were able to improve care processes that impact care. There was excitement and celebration, but also a humbleness that 6% is still not good enough. This is only the mortality rate for infants from Norwood discharge through the interstage period to Glenn surgery. Moving forward there will be a continued focus on this interstage time period but also working with clinicians who care for these infants during this earlier time frame to find additional ways to decrease mortality. It is always encouraging to see practitioners get excited about accomplishments and then get right back to work to find more ways to improve, especially when it directly impacts the care of your own child.
After the big news the focus shifted to a second main goal of the Collaborative, caloric intake. The discussion revolved around how centers document caloric intake and weight gain for all infants they see. Representatives from Advocate Children’s, Primary Children’s, and LeBonheur Children’s all shared ways that they track caloric intake and weight gain as well as who is responsible for doing so. Advocate Children’s tracks it like other vital signs like blood pressure and heart rate to give an example of the importance this has.
The call ended with a number of announcements. Nemours A.I. DuPont Hospital for Children in Wilmington, Delaware is the latest addition to the Collaborative bringing the total number of centers to 55. The fall Learning Session will be on November 7 & 8 in Cincinnati. The final announcement was that the Parent Page on the NPC-QIC website is under construction to help improve the resources available for parents. After that all signed off to get back to improving care with a heartfelt thanks from all of the parents!
Pink for Paul!
https://www.facebook.com/pink4paul
From time to time, we here at Sisters by Heart are approached with fundraising ideas, ways to generate awareness about HLHS and support Sisters by Heart at the same time. We are always so touched and honored when heart moms choose to support our efforts. We were recently approached with a new fundraising idea, borne out of one mother's unique way of showing love for her special HLHS son, Paul. We were so touched by her story, and thrilled to participate in this fundraiser, Pink 4 Paul. This is Paul's story, as told by his mother, Colleen. Please be inspired along with us, and read on to hear how you can support Sisters by Heart and go Pink 4 Paul this summer.
No one teaches us how to grieve. There are certain theories, support groups, quotes and passages that are intended to guide us and for some they provide solace and a road map and for others they provide simple words of encouragement. I think society has a need for people to hurry up and get better in the face of all different types of issues. People have a tendency to rush to support folks in immediate crisis- think of all the casseroles the day of a funeral but in aftermath, the days and weeks and months that follow, we tend to expect people to move on with their lives and resume normal functioning. After getting an HLHS diagnosis I was supposed to go through the Norwood (hard) get through the Glenn (easy) and then resume normal functioning until the Fontan. I wish I was one of those people who immediately became better and gained amazing life perspective in the face of life-threatening illness but I was not- I am not. That does not mean that who I am at my core and what I value deeply has changed it just means that in spite of myself I can get really worked up when it comes to HLHS.
For me, things went like this: I was happy, in denial and a little bit information crazy when Paul was first born. A few months in I was mad. His Glenn was supposed to be easy and it wasn’t. I was supposed to feel better about everything and I wasn’t- I was feeling…WORSE. More sad, more anxious, more in the weight of this diagnosis than ever before. I was sort of in a fog with little glimpses of hope during Paul’s first year of life. I checked his oxygen saturations constantly, we went to the doctor all the time, I researched vigorously for a cure, for someone- something to make it better. I got irrationally mad at our doctors and had moments of total denial. Looking back I can see this was all about grief- RAW grief. My little boy has a very different type of heart and there is no denying it. A shift happened in our family that caused my husband to be home with the kids much more. He was running the ship with me and he did it very differently that I had.
My husband is the coolest guy I know and has an amazing calm to him. He has the ability to compartmentalize in a healthy way like no one else I have ever known. That’s a good thing since I have almost every feeling all the time He taught me in the last year to see Paul as a little boy with a special heart, not as a ticking time bomb. He helped me see the forest for the trees so to speak. He helped me get through the fog in a way where the moments of joy started to over shadow the moments of panic. He didn’t sit me down and say “Colleen you should be feeling differently.” He just SHOWED me that parenting Paul was about parenting a little boy mostly and a heart kid sometimes.
Grief…What a word. Grief is an emotion that I will never lose in the face of HLHS but it is an emotion I have learned to manage. Here’s what I know right now- we have a beautiful two and half year old that can count to ten, knows most of his letters, is highly opinionated and really likes buddy fruit. We welcomed a little girl, Georgia Jane, on Valentines Day of 2014 and she is the queen of our little castle. Her heart is not perfect either, by the way. She has bicuspid aortic valve a very minor CHD but common for HLHS siblings (talk about re-visited grief but that’s a whole other blog). She is a sweet little ginger and Paul LOVES her. I fall more in love with my husband every single day. Our marriage is surviving and thriving in the face of this grief. It hasn’t been easy but we are making it, together. I have some amazing life long friendships because of HLHS and get to serve so many families by sitting with them in their pain and their grief when its needed. I am still who I was before HLHS. I have a huge crush on Gavin Degraw, get to work doing research for a lovely and highly patient company, I love to sing and dance, and I get an unhealthy joy from starbucks lattés and am a sucker for Lifetime television.
I wrote this blog about two years ago and I still mean every single word. The HLHS community is a beautiful place to unintentionally bloom. It has been a gift and gorgeous blessing to know these children and families. I love them as my own and follow their journeys with a lot of hope.
One of my best friends in the world is named Diana. Her little boy Jude is the first HLHS child I ever met. When I was pregnant with Paul, Diana and Jude and I met for coffee and conversation. I thought she’d arrive with a baby in a wheelchair on oxygen and IV drip; instead, she arrived with a big cheeked tow head with quite the personality. I fell in love with him and her that day and have been privileged to love them everyday since.
Most of you know that HLHS children appear “blue” pre-Fontan, especially in their fingertips and toenails. Diana shared an idea with me to paint my toenails blue when I was pregnant with Paul. She had done it for Jude, citing that as long as his toes were blue, hers would be too. At that moment, before he was born, I made a promise to Paul that as long as his toes were blue, mine would be blue and I have kept that promise for the last 2 and a half years, painting my toenails with every blue polish there is.
Paul will have his Fontan surgery on July 28, 2014 and hopefully his fingernails and toenails will be more pink. To show support and to raise awareness for congenital heart disease, we are asking folks to go Pink 4 Paul!
Paint your toes and/or nails pink. Post your picture on our facebook page https://www.facebook.com/pink4paul or Instagram #pink4paul and share with a caption of support. We will read all the messages to him during surgery.
You can purchase pink specific nail wraps and polish through our fundraiser with Jamberry Nails Independent Consultant Jenn W, between June 23rd and July 6th at www.jennw.jamberrynails.com. We have also made custom wraps that you can purchase by emailing JennWNails@gmail.com!! All proceeds will go to Sisters by Heart!
This is the best way I know to place my grief. In the face of this upcoming surgery, I am trying to choose acceptance and synthesis as a means to get through this time. During the Fontan, I expect to grieve, freak out, yell, ugly cry, laugh and smile, and maybe I will enter the fog again. As sure as the sun will rise, I will get out of that fog-no matter what happens, no matter how long it takes, I will live and breathe again. I will not be paralyzed by grief forever.
I write often about the space between in life, the power of each other, and the importance of love without condition. Maybe this is my lesson…these are my lessons in this journey. Whatever your process, wherever you are, however you grieve it's ok and it will BE ok. Thanks for fighting for HLHS and for allowing me to be with you on your journey, and you on ours as we sit with grief; we have so much hope. Paul is proof that the quality of life for a child with HLHS can be amazing and I hope he continues to be that proof throughout the rest of his long long long life.
Why There are “No Brothers by Heart”
The following post is brought to you by... two Heart Dads! Perfect timing for Father's Day.
A huge thanks to Travis Lewis and Trent Neely for their candid and honest thoughts and perspectives on being a heart dad and, as the title states, "Why There are no 'Brothers by Heart.'" So, who are Travis and Trent?
Trent, Avery, and Ellery
Trent Neely
Daughter: Avery (HLHS) - almost 3, Ellery (HH) - 5
Fontan: Scheduled for early July
Occupation: Teacher (Anatomy & Physiology, Health & PE)
Favorite kid activity: Being the tickle monster
Favorite ice cream flavor to share: Cookies & Cream
Lives in: Columbus, OH
Hospital: Nationwide Children's
Currently reading: The Tale of the Dueling Neurosurgeons
Favorite kids movie: The Goonies
Coping mechanism: Bad jokes
NFL Team: Bengals
Travis and Cael
Travis Lewis
Son: Cael ( HLHS) - just turned not so terrible two
Fontan: Scheduled for early July
Occupation: Physician Assistant and Athletic Trainer in a pediatric office
Favorite kid activity: playing outside
Favorite ice cream flavor to share: Moose Tracks
Lives in: Butler, PA ( just north of Pittsburgh)
Hospital: Children's Hospital of Pittsburgh
Currently reading: Any Given Monday
Favorite Kids Movie: Charlie Brown Christmas
Coping mechanism: Coffee
NFL Team: Steelers
Why There are No Brothers by Heart
by Travis Lewis and Trent Neely
Calling all dads… Calling all dads… Does anybody else hear crickets? It didn’t take long for us to notice a particular phenomenon in the heart community. Now we dads aren’t the most observant creatures in the world (unless we’re talking about fantasy football or baseball stats), so the observation had to be pretty obvious. Sisters by Heart has hundreds of affiliated moms, there are Heart Mom Facebook groups with 1,000+ female members, parent groups are predominately women, and a recent study about how to present a prenatal diagnosis had a 95% survey completion by the fairer sex. So, where are all the dads? And why is there not a support group like Sisters by Heart for Dads?
In order to understand this occurrence, it is important to first understand a few key differences between women and men. In this case, evolution is necessary to provide some insight. Historically, women have been the primary caregivers for children, and raising children is no easy task. As caregivers, socializing and bonding became an important survival technique; just ask any mom experiencing the terrible twos. Sometimes it feels as if a small army is required to attend to a child’s needs, and for help, many women turn to other moms. On the other hand, men are responsible for providing security and a source of nourishment. A group of men discussing their latest cave improvement techniques while hunting only tended to scare off the large animals they were hoping to bring home for dinner that night. As a result, we men tend to internalize more often.
This tendency of women to “tend and befriend” and men to “provide and protect” has resulted in variations in brain development of both men and woman. These variations can be coupled with the fact that women carry and then deliver a baby nine months later, while the male’s “job” could be a mere couple of minutes. In addition, males and females are socialized differently. Women are taught from a young age to be caring and compassionate and males are taught to be tough and emotionless. On the surface, we, the tougher species, appear to be devoid of emotions. However, this is hardly the case. We just deal with our emotions differently. Recent studies have shown that a Congenital Heart Disease diagnosis may hit the mom harder initially, but the stress tends to linger longer with dad. Because of their ability to socialize and bond, moms come to terms with the diagnosis faster and then shift their attention to how to care for a fragile infant. Dads unfortunately, do not typically reach out for help in the same way and often internalize the stress. As a result, the stress generally does not dissipate on it is own and may manifest itself in different forms for heart dads.
Another reason for the invisible nature of dad, is a result of one of the greatest powers in the universe. We all are exposed to it from birth, but we cannot fully appreciate it until we have children of our own. This super power is “maternal instinct” and it turns a regular, ordinary woman into SUPERMOM. We knew it as a child from our own mothers, but it isn’t until our wives or girlfriends step out of their hospital shaped phone booths with a baby that we truly begin appreciate this power. Seemingly regular women are rapidly transformed into an unstoppable force that has supersonic hearing, can soothe a crying infant, and change diapers with a single hand; all while sleep deprived. Regrettably, this metamorphosis can turn a new dad into a bubbling idiot only capable of putting baby formula into the coffee maker. This dynamic shift is rapid and extreme, frequently leaving dad in the back seat of the car that he is accustomed to driving.
As fathers of children with a complex heart defect, who still may not have appropriately dealt with the stress of the diagnosis, we are still scared and insecure about how to react. We too are thrust into this new situation and we want to do everything we can to help. However, it appears to come more naturally to mom. This is threatening to our masculinity, so we often do not exercise our ability to reach out for help. The last thing we want to do is make a mistake, because in this game, mistakes can be tragic. So we retreat to what we know - providing and protecting. When considering the idea of one parent choosing to stay home to care for a child, it is often mom. Dad continues to work in an attempt to make a larger financial contribution to the family. We feel this is our way to provide a sense of security for our family and to make up for all the shortcomings we perceive when compared to SUPERMOM.
So we ask again, where are all the dads? Well, in three of the social media groups that exist specific to dads, there are a grand total of less than 100 of us involved. This would make it appear that we all ran for the hills. Some do, but most go about winning their father-of-the-year award quietly. We take the kids to the doctor “because our wives told us to,” hoping to retain and deliver the correct information so we don’t have to tuck our tails. We go day to day holding onto similar stress and anxiety that moms do, but we don’t have the same social bonding ability to help cope with those feelings. The good news though is that the brain can change. Many dads are becoming more involved in the day-to-day care of their children. Although moms still hold onto a larger percentage of the primary care giver role, dads are beginning to do their share. Dads can also respond positively to bonding through social groups. Moms can help by encouraging their middle aged, balding child to reach out to other dads through social groups. This will help to reassure us that we aren’t the helpless creatures we feel like, knowing that we aren’t alone. Dads, join in the conversations, express emotions and ask questions. It may not be easy, but it will help. Maybe it will improve family dynamics or it might even get us out of the doghouse. Who knows, perhaps we’ll develop some of our own super powers…But we won’t know until we try.
What If…
Several weeks ago, Sisters by Heart reached out to our HLHS community asking families to submit photos of their heart kids with their care team members to be used in a special project. We are so excited to finally be able to share this special video project that debuted at the Spring National Pediatric Cardiology Quality Improvement Collaborative (NPCQIC) Learning Session!
The video features the song “What If” by Five For Fighting; to say the lyrics are powerful would be an understatement.
What If
It is safe to say we expected the crowd to react positively to the video, but what happened next came as a complete shock and truly moved the entire room (parents, cardiologists, nurses, dieticians, quality improvement experts, etc.) to tears. Dr. Gail Wright, upon watching the “What If” video, wrote down her raw, emotional thoughts to parents, then courageously read them to a room filled with nearly 200 participants:
What If….?
What if…
I told you we are not in control?
What if…
I told you that there are not answers?
What if…
I told you that I wish there was really a Journeyboard, rather than wide open space?
What if…
I told you I don’t know?
What if…
I told you I don’t understand why this happens either?
What if…
I told you I can’t make that part better?
What if…
I told you a bunch of knuckleheads won’t cough up the money to educate the nurses who are taking care of your baby tonight and that fighting for that is sucking the very marrow out of me?
What if…
I told you your life has changed forever today, but somehow you will keep walking forward?
What if…
I asked you how we can go forth together not knowing what’s going to happen?
What if…
I told you take a picture now in the CVICU so we can laugh together at his high school graduation?
What if…
I looked you in the eye and told you that your son is a miracle and is why I really do believe in miracles ?
What if…
I told you there are literally 300 people today who will be holding your baby in their hands with their focused attention and deepest intentions?
What if…
I tell someone that taking care of babies with half a heart has taught me how to live whole-heartedly?
Gail E Wright, MD
April 26, 2014
Upon viewing the “What if?” video by Sisters By Heart NPCQIC Learning Session
Cincinnati, Ohio
This - yes this - is a prime example of openness and transparency amongst parents and clinicians. These types of interactions and candid discussions will help reshape the way pediatric medicine is practiced. Parents and clinicians, coming together as partners, to move mountains. What better place to start than with pediatric cardiology? What better time to start than now?
Please feel free to share this post with your cardiac center leaders; let them know you're committed to working as a partner to transform the practice of pediatric cardiology on a broad scale.
Many thanks to Gail Wright - for taking a giant leap forward and improving upon our work together, as partners, to move mountains for HLHS children - and beyond.
HLHS Collaborative: March's Action Period Call
The National Pediatric Cardiology Quality Improvement Collaborative (NPCQIC) is preparing for its spring Learning Session - where parents and practitioners come together to discuss a range of topics and collaborate on how to transform care and identify best practices for HLHS infants.
If you've ever wondered what goes on backstage with NPCQIC, March's Action Period Calls focused on some of the "behind the scenes" work within the collaborative. The call began with details about the monthly NPCQIC e-newsletter received by participating cardiac centers and parents. There is some concern regarding the rate at which the newsletters are opened/read, however, each month, 80-90% of centers have at least one member utilizing the newsletter. Centers and participants discussed with NPC leaders how the information shared via e-newsletters might be more effective.
Conversation quickly shifted to planning and preparations for the Learning Session taking place April 25th and 26th in Cincinnati. Centers will be busy doing their homework to prepare and sharing tools that others can learn from.
Both practitioners and parents are excited for the upcoming Learning Session, as parent participation has nearly doubled in the last six months and the parent voice will be paramount to driving discussion. If you're an HLHS parent and interested in joining NPC-QIC Learning Sessions, please contact your cardiac center for details. A list of participating cardiac centers can be found HERE. If your center is not currently participating in the collaborative and you'd like to see their name on the list of "Participating Sites," please email stacey@sistersbyheart.org with your name and care center.
For parents attending the spring Learning Session, an orientation call will be held next week to help newly attending parents feel comfortable in NPCQIC's process and in working with dedicated groups of medical professionals.
For those who have attended a Learning Session in the past, please share your experience and for first timers, what questions do you have about what to expect? Not able to attend? Don’t worry, updates will be provided via Twitter, #NPCQICLS.
March's calls ended with an “unveiling” of the reorganized Collaborative SharePoint site. This site manages and stores NPCQIC's important information - tools that centers share and data for each participating cardiac center. The site is not available to parents - except for those on the Parent Leadership Team, but keeping with the theme of parent engagement, NPC involved a parent in the reorganization process. The site looks much cleaner and is easier to navigate.
While we don't always see "behind the scenes," there is much work going on within NPCQIC, all of which assists centers to collaborate and engage in improved care for our children.
We're very much looking forward to seeing many of you in Cincinnati in a few short weeks! Until then.... virtual heart hugs.
HLHS Collaborative: February's Action Period Call
February's Action Period Call updates are brought to you by Trent Neely and Rivkah Reichmann:
Action packed summarizes this month’s call! Each of the two calls began with a presentation of recent research derived from NPC-QIC's multi-institutional data set.
On Thursday's call, Dr. David Brown from Boston began with discussing a recent study regarding the association between Prenatal Diagnosis (PD) and Morbidity. Previous studies yielded variable results, indicating some benefits, as well as some downfalls. The recent data is now indicating more benefits to PD, such as decreased valve regurgitation, ventricular dysfunction, and shorter ventilator time post-surgery. One area that was not included in the study was parent stress. Parents were able to jump in and provide their experiences with PD and the ability to prepare for hospitalization and the interstage period.
On Monday's call, Dr. Matt Oster from Atlanta discussed a study regarding home monitoring. There was a discussion of some data on home monitoring. While the data reviewed didn't seem to correlate daily/weekly home monitoring with decrease in mortality or readmission rates, it did seem to impact weight gain. Those with daily home monitoring had better weight gain than those without home monitoring. The nurses and doctors on the call really wanted to hear from the parents -- they were interested in knowing whether home monitoring added to parents' anxiety and stress levels, or helped alleviate anxiety and stress. A good discussion was had of some of the benefits of home monitoring, and some of the challenges. The study, in particular, did carry it's own limitations, including omitting hybrid patients, excluding those with no echo data, and not having access center specifics.
Following discussion on these NPC studies, teams were updated on efforts made by the Research and Publications Committee. The Parent Leadership Team requested a summary of findings from a recent study on the relationship between Prenatal Diagnosis, birth location, and mortality. This is a valuable tool to help parents understand research studies. The first "Research Explained" can be found on the SBH blog and NPC-QIC's research page. Based on the response from this first review, NPC will continue "research explained." If you have come across a study or abstract relevant to HLHS and NPC's work, please feel free to email a link to info@sistersbyheart.org and we'll pass it along to the Committee. Additionally, NPC's Research & Publications Committee is adding two parent representatives to assist in reviewing manuscripts/abstracts and research explained projects.
Each call finished with review of survey results obtained from centers aimed at exploring various interstage practices. Some of the discussion surrounded center practices regarding red flags, interstage care, and frequency of follow up care. The discussion flowed into a discussion of reasoning behind frequency of visits and proximity to center. Some discussion was had regarding becoming more transparent in sharing data and protocols and the fortunate timing of NPC's new Transparency Workgroup.
According to parents on the call, February's AP Call was probably the most engaging call of the past year.
Please keep the discussion going by providing your thoughts and experiences on the following research topics:
Prenatal Diagnosis: Were you prenatally diagnosed? Was this beneficial to help you prepare or was it too much stress? How did either experience help you with care?
Interstage Monitoring: Did your center offer daily or weekly home monitoring? Did you find it helpful? More stressful? Less stressful? If you didn't have home monitoring, did you wish you did, or did you feel calmer without the stress of worrying about home monitoring?
Thank you for your continued engagement and your participation. Each comment shared improves the experience and outcome for future HLHS families. We look forward to meeting many of you at April's NPC-QIC Learning Session in Cincinnati!
Factors that Affect Survival of HLHS Infants
Often times, research studies are published in medical journals that relate to our HLHS community. Some of these studies spread rapidly through social media sites and become a topic of conversation amongst HLHS parents.
At the request of NPC-QIC's Parent Leadership Team, their Research and Publication Committee reviewed a recent article that gained quite a bit of traction with HLHS families, nationwide. The study was published in the October, 2013 edition of Circulation: “Prenatal Diagnosis, Birth Location, Surgical Center, and Neonatal Mortality in Infants with Hypoplastic Left Heart Syndrome.”
NPC-QIC's Research and Publication Committee reviewed the study and provided the following summary for parents, or "Research Explained" as we like to call it.
Key Findings: Prenatal Diagnosis, Birth Location, Surgical Center, and Neonatal Mortality in Infants with Hypoplastic Left Heart Syndrome
_________
The journal Circulation published a study in October 2013: “Prenatal Diagnosis, Birth Location, Surgical Center, and Neonatal Mortality in Infants with Hypoplastic Left Heart Syndrome.” http://circ.ahajournals.org/content/early/2013/10/17/CIRCULATIONAHA.113.003711.abstract
The NPC-QIC Research and Publication Committee has reviewed this article and a summary of the findings can be found below.
Main Finding from this Study:
The authors of this study concluded that infants with HLHS born closer to a surgical center that performs cardiac surgery on infants have a higher survival rate than infants born far from a surgical center.
About this study:
Why is this study important?
Over the past several devades there has been dramatic improvement in surgical survival in infants born with HLHS. However, ~20% of infants born with HLHS still die within the first months of life. We are constantly looking for ways that we can improve the survival of infants with HLHS, trying to identify improvements we can make in the way we care for these infants. This study attempts to identify risk factors that we might be able to address to improve this survival.
How was this study performed?
The researchers in this study used information from the Texas Birth Defects Registry and identified 463 infants with HLHS born in Texas from 1999-2007. The researchers then looked at where these infants were born, and what the distance and driving travel time was between their birth hospital and the closest surgical hospital that performed stage 1 surgical palliation (Norwood procedure). The researchers then looked for a relationship between this distance and the likelihood of survival of these infants.
What were the results of the research?
Data for a total of 588 infants with HLHS born in Texas between 1999-2007 was available in this Registry.
Several factors were found to be associated with better or worse survival for infants born with HLHS:
The researchers concluded that infants born far from a surgical hospital (more than 90 minutes driving distance away) have worse survival.
Infants with a birth weight <2.5 kg had worse survival.
Infants who had surgery at a surgical hospital who performed more Norwood surgeries had slightly better survival after that surgery.
While prenatal diagnosis was not by itself associated with better or worse survival, prenatal diagnosis is a very important factor related to distance from the surgical hospital; 66% of infants who were born less than 10 minutes from the surgical hospital were diagnosed prenatally as compared to only 13% of the babies born more than 90 minutes from the surgical hospital.
What are the limitations of this study?
Studies that use databases like the Texas Birth Defects Registry are nice because they allow researchers to look at a large number of patients. This is especially helpful when trying to learn about patients with rare problems like HLHS. However, one of the problems with research using databases is that there often is incomplete information about the patients. The following are some of the other things that limit the interpretation of findings from this study.
Survival was better in infants born in the more recent time period (2003-2007) than in the older (1999-2002) period. More infants were diagnosed prenatally in the more recent time period (49% versus 25.5%) and that number has likely continued to increase in recent years.
More infants living more than 90 minutes from the surgical center were Hispanic (30% of mothers born in Mexico) and lived in poverty, suggesting they may have had more limited access to care, including lack of prenatal diagnosis. These socio-demographic factors were not included in the study of factors that may affect survival.
What are the takeaway messages considering the results and limitations of the study?
There are many factors that affect survival of infants born with HLHS. There are some findings from this study that may allow us to improve survival of these infants moving forward.
This study did note worse survival in infants with HLHS born far from surgical hospital. However, there are likely other factors that influence that finding, including the changes in surgical practices over time and socio-economic factors that may influence survival.
Prenatal diagnosis is important because it may reduce mortality if mothers living far away can deliver close to a cardiac surgery center. Prenatal care is also important because we know that infants with HLHS who are born prematurely or with a low birth weight (<2.5kg) have worse survival. We should be doing everything we can to make sure that pregnancies receive adequate prenatal care and appropriate referrals.
We need to continue to understand the relationship between surgical volume (the number of specific procedures that are performed at a surgical hospital) and the survival before and after surgery in infants with complex heart problems like HLHS. Some studies, including this one, have suggested that the more surgeries that are done the better the survival. Collaborative work, like that going on in NPC-QIC will be required to understand the answer to this question.
Shopping for a Cause
Heart Week is coming to a close today but if you are still looking for a way you can give back during Heart Month check out one of these fundraisers we have going on right now.
You can help out Sisters by Heart and get yourself a great gift at the same time. One of our board members, Kathy Baker, is hosting a Virtual Younique makeup party. A portion of the proceeds from every purchase will be donated to Sisters by Heart.
Younique is known for their mineral pigments and their AMAZING 3D fiberlash mascara. If you have ever used Bare minerals, Younique has similar products. The mineral based makeup is free of chemicals and not only looks great but feels great too. What is even better is you can stay in and shop from your couch in the comfort of your own home. If you are having a hard time deciding what to get, check out the "Browse Looks" section of the site for many user uploaded photos. Find more ideas on Pinterest by searching Younique makeup. The mineral pigments can be used wet or dry or a combination of both. Play around and see what look you like best.
If you purchase a collection, you not only save 25% but you will also receive a FREE lipgloss or Mineral Shade. This is a special offer Kathy is running so it won't appear at checkout. If you order a collection, email Kathy at info@sistersbyheart.org and let her know your name, address and what shade of gloss or pigment you would like.
The virtual party ends on February 17th.
Click the link below to start shopping!
https://www.youniqueproducts.com/ChevaIsing/party/61019/view
A Heartfelt Donation: eBay Foundation
Sisters by Heart is thrilled to announce that we've been the recipient of an eBay Foundation grant!
One of our Sisters by Heart board members, Stacie Jackley, has been working for GSI Commerce, a subsidiary of eBay, inc., for the past 11 years. A few months ago, she received an email from the eBay, inc. GIVE Team offering a unique opportunity for employees to apply for a grant up to $5,000 to support their favorite non-profit organization.
Stacie immediately thought of Sisters by Heart and, along with fellow board members, completed the application. The application was submitted with fingers crossed.
We found out in late December that Sisters by Heart was one of the organizations to be awarded a grant of an astonishing $5,000! Needless to say, we are ecstatic and so appreciative of the generosity of the eBay inc Foundation! Sisters by Heart has grown tremendously since established in December 2010 and we're thrilled at how this grant will help us further our mission of supporting families facing a new HLHS diagnosis!
Kellen Jackley (2 years old, HLHS) presenting the grant check to Sisters by Heart
The GIVE Team aims to engage employees through volunteerism and by making charitable grant recommendations. Employees have the opportunity to recommend a Non-Profit Organization they are passionate about and would like to help fund their cause. The GIVE Team committee then works together to review the recommendations to determine which organizations receive funds based on a number of factors including financials, potential impact, and need.
Each year, eBay Foundation provides grants of more than $2 million USD to support organizations that promote economic and social well-being, making more than $23 million USD in grants since its first year. But while the Foundation provides generous monetary support, eBay Inc. GIVE Teams, made up of employee-volunteers, further the Foundation’s mission and bring the company’s values to life.
eBay Foundation GIVE Team grants are awarded by the eBay Foundation Corporate Advised Fund at Silicon Valley Community Foundation.
Thank you a million times over GIVE Team and eBay inc Foundation for awarding us this grant - and Stacie Jackley for nominating us! Your generous contribution will help support our mission to provide HOPE to hundreds of families who are facing the devastating heart defect, Hypoplastic Left Heart Syndrome (HLHS), and a lifetime of care for their child.
Research Opportunity: Prenatally Diagnosed Moms Need Apply!
As you can imagine, we welcome and receive constant feedback from HLHS families across the country. Recently, Miami Children's Hospital referred one of their families to Sisters by Heart. We're so very glad they did, as there is a unique opportunity for single ventricle families to participate in a research study.
Dawn Silverman, a heart mom with a passion for psychology, took her education to a very different level than she thought possible, after her unborn son, Caden was diagnosed with HLHS. Dawn decided to use her psychological training and her experience as a heart mom, to advance patient centered research in the Congenital Heart Community.
Significant focus on patient centered and driven research makes Dawn's study unique - she is literally the patient and the researcher! What better way to encourage patient driven research than helping Dawn reach hundreds of single ventricle families.
Psychology Doctoral Study - Dawn Silverman, LMHC, MEd/Eds
The Lived Experience of Pregnancy with a Neonatal Diagnosis of Single Ventricle Heart Defect: A Heuristic Study.
The purpose of Dawn's study is to investigate the prenatal experience following the diagnosis of a single ventricle fetus.
The following is a layout of some of the study criteria, procedures and requirements for HLHS families to participate. Sisters by Heart believes that nearly all prenatally diagnosed families we serve will meet the study criteria. The committment to participate is small, but may carry significant benefits to future HLHS moms.
Participant Criteria: Mothers who were informed during their pregnancy that their baby had a single ventricle defect, and whose baby/child with the heart defect is still alive. During that pregnancy, you had to be pregnant with just one baby and received the congenital heart defect diagnosis while you were pregnant (not after the baby was born). All participants will be between at least 18 years of age.
Study Procedures
Participants will meet with the researcher for 1 to 3 hours to be interviewed about their pregnancy experiences.
Interviews will be recorded.
All recordings and information will be kept confidential with no use of participants’ identifying information.
The recordings will be transcribed and analyzed by the researcher.
Participants will be provided with a summary of their interview (via phone or email) to verify that it is an accurate description of their lived experience.
A report regarding the findings from the analysis will be generated.
Benefits: For this study, you may benefit from potentially gaining greater insight into your pregnancy experience. Participants may also gain a level of satisfaction and sense of “paying it forward” by knowing that their participation will also offer a greater benefit to the scientific community. The data participants impart can yield information that can potentially help decrease the suffering of other women who are actually living this experience as well as serve to assist healthcare workers to better meet the emotional needs of the pregnant women they treat.
Time Commitment: Participation requires about 1- 3 hours. The interview will be conducted at a mutually decided upon secure location. Participants will also be provided with a summary of their interview to verify that it is an accurate description of their lived experience over the telephone or via e-mail. This will require less than an hour of the participant’s time.
Enrollment: To enroll, interested participants should contact the researcher via email (dsilverman@capellauniversity.edu). The researcher will email additional information about the study and eligibility requirements. Women meeting participation requirements will then be emailed information about how to consent to participate in the study. Once your questions are answered, enrollment requires a signature consenting to participate.
Contact: If you are interested in participating or for additional information, please contact Dawn Silverman at (561) 329-3871 or dsilverman@capellauniversity.edu.
Additional information regarding Dawn's study can be found on her research site: https://sites.google.com/site/chdstudy/home
Thank you Dawn, for your passion and empathy for heart moms and in dedicating your doctorate work to improving the prenatal experience post single ventricle diagnosis. We look forward to reading a summary of your study results once your dissertation is complete!
HLHS Collaborative: December's Action Call
As mentioned last month, Sisters by Heart will be providing a summary of the dialogue (involving both clinicians and parents) during the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) Monthly Action Period Calls.
For December, the action call began with an update on a newly formed Collaborative work group - a Transparency workgroup. With great interest in Transparency, invitations were sent to approximately 15 cardiologists, nurses, and parents. Most encouraging, this group will likely be comprised of a 50/50 split between health care professionals and parents. The first objective of the Transparency group will be to discuss short and long term goals, legal matters, and then develop an update for the Spring Learning Sessions in Cincinatti. The initial goal for centers involved in the collaborative will be to share data amongst themselves in order to drive quality improvement at a more rapid pace. Co-leaders for the transparency work group are: John Kuglar (cardiologist) and Stacey Lihn (parent).
The call also focused on a review of requirements for centers to maintain certification in the NPC-QIC and how data collection forms were modified to help streamline collected data. The data collected is the vital for the work that the collaborative does and a great deal of work goes into collecting the most appropriate information.
The main topic for December's call was Growth during the Interstage period. Growth of babies during this period is one of the vital pieces of data centers are using to help determine health and success of their patients. Centers implementing interventions, such as using scales at home, conducting a feeding evaluation, and providing red flags to parents, experienced improved growth of infants that they cared for. Centers used to think that HLHS babies just didn’t grow during the interstage. Through the work of the collaborative, centers don’t accept this notion anymore. December's call ended with a highlight of some of the work centers are doing to improve interstage growth.
Thanks again, Trent Neely and all parents who participate on the monthly Action Period Calls for providing input, taking notes and preparing summaries for the HLHS community.
Growing Up with HLHS
During the National Pediatric Cardiology Quality Improvement Collaborative's 2013 Winter Learning Session in Cincinnati, Sisters by Heart Board Members had the opportunity to meet Diane Pickles, mom to Jake, a 19 year old living with HLHS. Diane offers great insight as a veteran HLHS mom, and even greater, Jake's personal insights on growing up with HLHS.
Diane and Jake have graciously granted us permission to share their journey over the past 19 years. And Jake, well, he's allowed us to share with our families, his college essay:
Jake and Diane Pickles
To look at me, you would never guess anything was wrong. The truth is, however, that I have quite a story. I look like an everyday high school student, but I’m really not.
I was prenatally diagnosed with Hypoplastic Left Heart Syndrome. This means that while my mother was pregnant it was determined that I had only one of the heart’s two ventricles. In layman’s terms, I have half a heart. My parents were told that my odds of survival were quite low and if I did survive, I would have poor quality of life. One doctor even told them to terminate the pregnancy. My parents thankfully decided to have their second son. They knew I would face obstacles in life, but they prayed I would be able to overcome them. My supportive family welcomed me into the world on September 2, 1994.
I have had three open heart surgeries – the first at three days, the second at six months, and the third at two years. While I don’t remember my operations, I have been told they required a lot of strength and courage to survive. In addition to my surgeries, I have had four cardiac catheterizations, many tests and procedures, and more doctor visits than I could count.
Throughout my life, I have coped with frequent infections and chronic asthma. I have had several hospitalizations and many trips to emergency rooms as a result. Once while in the hospital, we did the math and determined that I have spent more than one hundred nights at Boston Children’s Hospital. I get sick much more frequently than my peers. I have been sick with obscurities such as swine flu (which required a week in the hospital and missing my 8th grade graduation), c-difficile, and erythema multi formae. Most recently, I was hospitalized for a week with pneumonia.
Due to these chronic illnesses, I have faced significant challenges academically. I have missed large amounts of school, and I have also spent many days in school feeling quite ill. When I return to school, I am lessons behind my classmates and struggle to catch up. Early on, I missed a lot of the “basics” and important foundations which has caused challenges in subjects like math and English. Though I don’t dwell on them, I face non-academic day-to-day challenges as well. My friends are very athletic where I am not which has made it difficult to keep up with them in sports and activities. Many of them play organized sports like football and hockey which I am not able to play. I get tired more easily than most teenagers which is a challenge at work and at school.
My personality has helped me overcome these obstacles, particularly my sense of humor and positive outlook. I remind myself often that my challenges could be much worse. I have seen what other cardiac kids experience, and I am thankful that my problems aren’t as severe.
I may have half a heart, but my life is full.
Sisters by Heart asked Jake's mom, Diane, an incredibly thoughtful and genuine individual, to share the HLHS journey from a parent perspective, from birth through teenage years. She's given so many pearls of wisdom in this post and we're so thankful to Diane for sharing.
By Diane Pickles
There is so very much that I could share about the last 19 years of raising a child with HLHS. Although Jake is not the oldest survivor, he is certainly on the oldest end of the survival spectrum. I know that a great deal has changed in 19 years, though the most important aspect hasn’t, unfortunately, changed at all – it is still heartbreaking, exhausting, and frightening to have a child with HLHS. But there’s one more incredibly important thing that also hasn’t changed – the love of a parent combined with the determination of these amazing kids can overcome all kinds of obstacles.
The first 2 years of Jake’s life are a total blur. Somehow, we moved through the chaos and stress and got to the other side. And what I found on the other side, particularly as Jake reached school age, was a challenging transition -- from medical management of HLHS to emotional, social and developmental management – on top of the medical issues. It has been the part of our journey that has challenged me the most. I’m not saying that getting through Jake’s surgeries was easy – because God knows as do each and every one of you that it was incredibly difficult. Nor has it been easy to deal with frequent infections, severe asthma, emergency room visits, ambulance rides, and admissions from the age of 2 onward. But the non-medical “stuff” that has gone along with Jake’s disease was, in many ways, much more difficult. It was certainly not easy to watch our child in physical pain – but most of the time, there was medication that could be administered to ease that kind of pain. Other types of pain were much, much harder.
Jake desperately wanted to play baseball, but the coach wouldn’t play him because he was slow around the bases and not as strong as his peers. He struggled mightily to keep up in school given learning issues, compounded by frequent illnesses, and had more than one teacher call him lazy. Doctors constantly told our one time failure to thrive child that he needed to lose weight. Jake missed many special events, parties, and graduations. Each of these things made him sad, frustrated and angry. I worried about his self-esteem, his report cards, his morale, and his social life. Sometimes I still do.
There are no prescribed treatments for these situations. And they are difficult. Challenging. Sad. You struggle to prop your child up while feeling heartbroken yourself. What I think is essential, and what I tried to do through each of these struggles, was to acknowledging Jake’s frustrations without allowing him to wallow in self-pity. I’ve tried to strike a balance between acknowledging that things may be harder than others for him while pushing him to do his best. Sometimes that was much easier than others. We have tried to raise Jake with courage, grace, dignity, and optimism. When you live with a life-threatening disease like HLHS, there are likely to be non-physical challenges that go along with the disease. For some, they are academic; for others they are emotional; for others they are developmental; and for still others they are social. Sure, lots of kids without HLHS face these kinds of struggles as well. But I think that for a child living with a disease like HLHS the childhood, adolescent, and teenage struggles are frequently filled with these kinds of struggles. And when you’re dealing with that in addition to a serious medical condition, it’s a lot on the plate.
Like each of you, I grieved when Jake was diagnosed and through each of his surgeries. I had to grieve the loss of a normal, healthy infancy and childhood for our second son. And each time I have seen Jake feel limited, frustrated, or down about himself because of his heart disease, I have grieved all over again. For me, one of my greatest challenges as the mother of a child with HLHS has been to avoid letting my own grief about Jake’s struggles color his interpretation of his world. Sometimes I have succeeded at that, and sometimes I’ve missed the mark. Parenting is an art, not a science – right?
Perhaps the greatest words of wisdom I can offer from 19 years of HLHS are these: You are stronger than you think and so is your child.
We have been incredibly, wonderfully blessed with an amazing kid. Jake is outgoing, personable, funny, well-liked, and happy. He is currently a freshman living away at college, loving the experience and working hard in the classroom and at his job. He gives himself weekly immunoglobulin infusions in the common room of his dorm and doesn’t care who sees his scars. He matter-of-factly told his boss that he might need to take a rest if they’re doing something really physical but that he’d more than carry his weight. His friends know he has half a heart but don’t seem to give it any thought at all. He has tons of friends, tons of confidence, and an amazing outlook on life. His struggles aren’t over, and there are still times (as recently as last week, in fact) when I grieve all over again in the face of his difficulties. But as we recently told Jake, when it comes to some of the biggest challenges of all, he has hit it out of the park. He is a survivor.
You will continue to be utterly amazed by your HLHS child’s courage and capacity for love, empathy, and joy. I won’t lie to you: It will be hard. Some days, just like the early days of HLHS, will be really hard because you will see your child’s social, emotional or developmental life impacted by their heart disease. You will be sad, you will be frustrated, and you will be angry that your child has half a heart. But you know what? You’ve got what you need to handle it and so does that amazing, courageous, miraculous HLHS child of yours.
Trust yourself and your capacity to raise a survivor. You’ve got this.
A huge thank you to Diane and Jake for sharing your journey, wisdom and insights into Life with HLHS.