Interstage Care and Mortality (surgical v. non-surgical sites)
Special thanks to Dr. David Schidlow
The journal, Pediatric Cardiology, published a study in August, 2014: Site of Interstage Care, Resource Utilization, and Interstage Mortality: A Report from the NPC-QIC Registry. This study was completed utilizing data from the National Pediatric Cardiology Quality Improvement Collaborative patient database.
The abstract can be found at the following link: http://www.ncbi.nlm.nih.gov/pubmed/25107545
What is the background of this study?
o Medical problems and early death remain a problem for children with hypoplastic left heart syndrome (HLHS) during the outpatient “interstage” period between the first (Norwood) and second (Glenn) operations.
o The National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) identifies differences in the care of interstage patients in the hopes of learning the best way to care for these children during this sensitive time.
o One difference in care is the place where children receive interstage care. Some are cared for at the surgical site (SS) that performed the Norwood operation. Others are cared for at a non-surgical site (NSS), which could mean a hospital that does not perform the Norwood operation or a private cardiologist. Among those who are followed at a NSS, the distance to the surgical site can vary greatly.
The aims of this study were to answer the following questions:
o Where do HLHS patients receive their interstage care? The surgical site (SS) that performed the Norwood operation, a non-surgical site (NSS), or at a combination?
o How far is the NSS from the SS for those children who are followed at a NSS or at a combination of sites?
o Are there differences in the number of medical problems or deaths associated with the site of interstage care and/or the distance from the surgical center?
How was this study performed?
o The researchers looked back at patients with HLHS entered into the NPC-QIC database over an approximately five-year period (July 2008 to February 2013). The site of each patient’s interstage care was noted as (1) the SS that performed the Norwood procedure, (2) a NSS as described above, or (3) a combination. The distance from the SS to NSS was identified for patients in categories 2 and 3. The number of interstage medical problems, emergency department (ED) visits, readmissions to the hospital, and deaths were identified for each of the three groups.
What were the results of the research?
o Most patients (60%) received their interstage care at the SS. The remaining patients received their care at a NSS (17%) or at a combination of sites (21%).
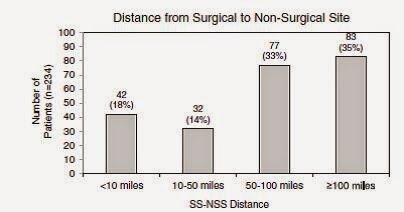
o The patients who received interstage care at a NSS or at a combination of sites were followed at a variety of distances. A large number (68%) of those patients were followed at a distance of 50 miles or greater from the surgical site. The following figures are taken directly from the paper.
o Patients followed at the SS were more likely to have emergency room visits and readmissions. Conversely, patients followed at a NSS or at a combination of sites were more likely to have problems identified with breathing and/or feeding.
o Despite these differences, there were no differences in the rates of death or in the reasons for death among the three groups. Similarly, there was no difference in rates of death based on the SS-to-NSS distance.
o There were 66 patients, approximately 10% of the entire group, who unfortunately did not survive the interstage. It was notable that among those 66 patients, 37 (55%) percent of them died in their home or in an emergency department.
What are the limitations to this study:
o There were several limitations to this study. The main limitations related to the level of detail that was able to be ascertained about these patients.
o The NSS and combination categories were very broad. As noted above, they could be anything ranging from a large medical center that simply does not perform Norwood operations to the office of a single practitioner far from a medical center. This study could not distinguish smaller differences between the two.
o The significance of more breathing and feeding problems identified at the NSS or combination is unclear. It is not known if these patients truly had more problems, or if the fact that these problems were identified reflected more vigilance on the part of the caregivers. Another limitation is that these categories are very broad. Feeding and breathing problems could mean different things to different caregivers. This lack of detail makes a refined analysis somewhat difficult.
What are the takeaway messages considering the results and limitations of this study?
o The site of interstage care does not seem to affect the likelihood of a patient passing away during the interstage period. Similarly, the distance of interstage care from the SS that performed the Norwood does not seem to affect the rate of death.
o More ED visits and readmissions occurred in the SS group, and conversely, more feeding and breathing problems were identified in the NSS and combination groups. As noted above, these differences did not seem to have an effect on death.
o Finally, the mortality rate still remains high at approximately 10%, with many patients dying at home or in an emergency department. This is an important reminder that we still have room to improve interstage care and decrease mortality.
If you missed the first three installments of Research Explained, you can link to them here: https://www.jcchdqi.org/research