Take Action: Be Part of the Solution
Over the last year, Sisters by Heart has played an active role in the National Pediatric Cardiology Quality Improvement Collaborative (NPCQIC). NPCQIC's goal is to improve the quality of care and outcomes for HLHS infants, particularly during the interstage period. Learn more about NPCQIC's goals and visit the "Parents" tab here: https://jcchdqi.org/.
Twice a year, NPCQIC holds Learning Sessions for the 50+ cardiac centers across the country to attend and share their practices, successes, procedures, and ideas. Over the last 12 months, with Sisters by Heart's help, parents played a much more active role in the NPCQIC learning network. The network is made up of cardiologists, nurses, dietitians, quality improvement researchers and parents of HLHS children. We all come together to have candid conversations about feeding, mortality and the struggles we face as parents and clinicians.
One major boundary both clinicians and parents noticed in the pediatric congenital heart community is a communication gap. This large gap (acknowledged by almost everyone involved in the collaborative) exists between two of the most important players on the team - the parents and the cardiac clinicians. As you know, there's little room for miscommunication in the HLHS world.
By invitation from collaborative leaders, Sisters by Heart is actively participating in NPCQIC to bridge this communication gap - so that parents and cardiac teams are working as one. Sisters by Heart board members attend the Learning Sessions each fall and spring and participate in monthly telephone conferences with cardiac centers. As HLHS parents, we're working to empower all parents to play an active and vital role in our child's care; you know your child the best and your cardiac team lacks something every parent is blessed with - parental intuition.
Aside from the Learning Sessions held in Cincinnati each spring and fall, NPCQIC holds Monthly Action Period Calls. Parents engaged in the collaborative participate in these calls - sometimes to listen, sometimes to teach. There is limited space for these Action Period Calls, however, Sisters by Heart wants to make certain that all HLHS families are provided information on what is being discussed and who they can contact to get involved in the broader discussions.
The November Action Period calls included the following information/discussions. A special thanks to HLHS dad, Trent Neely, for providing this update:
Three new cardiac centers were added to the collaborative: Baston Children's, Children’s Hospital of Alabama, and Rainbow Babies & Children’s Hospital. The Collaborative is now made up of 54 centers across the country, meaning that over 90% of the centers performing HLHS palliation are involved with NPCQIC. It is very encouraging how open these centers are, working together to improve care for HLHS infants. With the new centers joining the call, an overview of how data is gathered, charted and discussed was given. Each center can view their own reported data and their relationship to how the other centers in the collaborative are performing.
The main topic of conversation during the November Call revolved around data transparency amongst centers. At the Learning Session in September, after reviewing successful transparency models from other national pediatric collaboratives, there was overwhelming agreement that NPCQIC centers should move towards transparency within the collaborative - so that other centers can see outcomes being attained amongst their peers. All parents on the calls and at the Learning Sessions supported a move to transparency; it is our belief it's the fastest way to "move the needle" on quality and improved outcomes.
There is definite momentum growing in the transparency movement and it appears as though NPCQIC is ahead of the curve on the topic. The next step in transparency is the formation of a "Transparency Workgroup" which will include parents, clinicians and possibly cardiac surgeons. Rob Beekman, M.D. also shared a TED Talk about transparency which embraces the "What Doctors Can Learn from Each Other" discussion.
If you'd like to learn more about the National Pediatric Cardiology Quality Improvement Collaborative, please email Kay Fricke, NPC's Parent Liaison at Kay.Fricke@cchmc.org. The collaborative's next Learning Session will take place April 25-26th in Cincinnati - so mark your calendars! We'd love to see more and more SBH families (moms and dads) involved in transforming the lives of HLHS infants and children.
"If everyone is moving forward together, then success takes care of itself." ~ Henry Ford (the second paragraph in this link is of particular poignancy - the Life of Henry Ford).
“Unity is vision; it must have been part of the process of learning to see.” ~ Henry Adams, The Education of Henry Adams
Remember, our voices are meaningful, our voices are needed.
A Mother's Perspective: The Other Sibling
If you follow our Facebook page, you may have seen last week that one of our Board members, Amy, had an incredible experience with her HLHSer, Bodie. Last weekend, Bodie had the opportunity to be the honorary captain of the Cal Poly Mustangs football team in San Luis Obispo, CA. If you haven't read his story, you can find more about it in this touching article here.
In addition to honoring Bodie, the Mustangs also honored Amy's older, heart healthy daughter, Sierra. We asked Amy to share a little of what led up to the decision to include Sierra in the evening.
----
Last week, I chaperoned a fieldtrip with my daughter's 1st and 2nd grade class. As I listened to the peels of laughter coming from the middle row in my minivan, I tried to put my finger on what made those girls different than my sweet Sierra, sitting in the back row with one of her best friends, quietly talking and coloring. After much thought, I realized what it was. The girls in the middle row had a complete self-absorbed love of life so inherent in most 6 and 7 year olds.
Sierra, at 6 1/2 is, for the most part, happy. She is well adjusted. She loves school and has friends. She's joyful. But it's different than her peers. She doesn't have that wild-eyed innocence of youth, where the world is at your doorstep, and all opportunities abound. The innocence that allows one to forget all else and scream and shout in pure joy over the newest song or toy.
She has an empathy not usually seen in children her age. But there is also a heaviness about her. Her teacher has noticed it. My brother-in-law commented on it when he was visiting. I suppose that innocence was lost somewhere between being a precious 3-year old with a younger brother born with 1/2 a heart and confined to the hospital for 5 months...and being a first grader whose recently post-Fontan brother's course was so complicated that she never knows at the end of the day whether mommy will really be the one to pick her up...or whether mommy and brother will be at the hospital again and someone else will be picking her up. The uncertainty of this journey is hard for me...and I've had 37 years of life lessons to help me weather this storm. She's had 6 1/2. I can't even fathom how hard this is for her.
Parenting an HLHS child is hard. Parenting an HLHS child alongside a heart-healthy siblings is even harder. And when that HLHS child has complications, it borders on impossible. There is always such a tenuous balance to maintain, between focusing on your medically fragile child and other siblings.
The ebb and flow of caring for an HLHS child in particular adds to the complexity, I think. There are parts in this journey where you are in nothing but survival mode. Times where it is all you can do to focus on your HLHS child and getting through the day. Those are seasons where you have no choice but to rely on family and friends to share the burden in caring for your healthy children.
And then, for most HLHSers, there are seasons of rest. Seasons where life shifts back into a normal rhythm and your focus can be more evenly distributed. For our family, the first year was the roughest. And then we shifted into more or less normal rhythms. But the last few months have been exceptionally rough again, as we found ourselves unexpectedly thrown back into survival mode, when my son encountered complication after complication from his Fontan, including an additional open-chest surgery, low oxygen saturations, arrhythmias, a staph infection at his pacemaker site, and ultimately an interventional catheterization.
He is much more stable now, thankfully, and our delicate balance is slowly shifting back again. We are working on healing the hurts caused to his heart-healthy sister during that time. The survival mode was necessary, but the damage it leaves cannot be ignored.
So, when Bodie was invited to be an honorary captain of the Cal Poly football team, we were honored and humbled. But, my next question was whether Sierra could also be involved somehow. It was an awkward request, but in my mind, a necessary one. Sure, she hasn't gone through the physical aspects of this journey, but her world has been every bit as rocked. Her scars may not mark her chest, but they're just as deep.
And so we don't celebrate Bodie unless we can also celebrate Sierra's part in this journey. And sometimes that means saying no to amazing opportunities. This time, because of the generosity of some absolutely incredible people, it meant saying yes to an even better opportunity. While Bodie got to be the honorary captain, Sierra got to be an honorary cheerleader.
She got to lead the cheerleaders down the hill before the game. She got to stunt with the cheerleaders. She got to hold their signs. She was so proud. SHE was the shining star.
It was the perfect step on our path toward healing. And one we will cherish for years to come.
As difficult as it may be to ground yourself in this journey with HLHS, the majority of us recognize the impact on our heart healthy children, the siblings to our HLHSers. Our advice? Keep them at the forefront of conversations, the forefront of planning. Make them a part of the HLHS journey. Allow them to control situations when possible, give them choices - for they've likely not been given much allowance in that regard while you're in survival mode. Be mindful of their own unique HLHS sibling journey. And, when possible, make today and tomorrow about them. Focus on their strengths and find moments for them to shine - because they will shine and they'll knock your socks off.
A Unique Opportunity with What to Expect
As part of SBH’s ongoing mission to create awareness for all CHDs, we jumped at the opportunity to guest blog for What to Expect (WTE) to help educate and empower thousands of expecting readers!
As a first-time mom pregnant with my daughter, I never considered the possibility that my baby wouldn't be born 100 percent healthy. I was never nervous going in to an ultrasound or concerned when additional ultrasounds were scheduled. I assumed everything would be routine. When I was 31 weeks pregnant I learned that "routine" was not my reality. My daughter was diagnosed, in utero, with a critical congenital heart defect called Hypoplastic Left Heart Syndrome (HLHS), which essentially meant she would be born with half a functioning heart. That day (and every day since) my eyes have been opened to a whole new world that I didn't know existed..
Congenital heart defects (CHD) are found in approximately 1 in every 100 live births in the United States. CHDs range in severity — some requiring immediate surgical intervention after birth and some may only need monitoring as the child grows into adulthood. Regardless of severity, the key to increasing survival rates and decreasing complications in children born with CHDs is early detection and diagnosis.
The first opportunity for diagnosis is through pre-natal ultrasound. Detection is not always possible during anatomy scans however here are a few questions you can ask your sonographer for a more in-depth look at your baby's heart (provided by Boston Children’s Hospital)
1. Do you see 4 chambers in the baby’s heart?
2. Are there two upper chambers (left and right atria), each with a valve controlling blood flow out of them?
3. Are there two lower chambers (left and right ventricles), each with a valve controlling blood flow out of them?
4. Do the two vessels leaving the heart (aorta and pulmonary artery) cross each other as they exit?
5. Is the wall between the two lower chambers intact, without any holes?
6. Is everything else in the heart normal?
If the sonographer is uncertain or replies no to any of the above questions, ask your OB to refer you to a fetal cardiologist as soon as possible.
If the sonographer is uncertain or replies no to any of the above questions, ask your OB to refer you to a fetal cardiologist as soon as possible.
The second opportunity for diagnosis is at birth. Many babies with CHD are born with no signs or symptoms of a heart defect. My daughter scored a 9/9 on her APGAR. Had we not known about her fatal heart defect before birth she could have fooled us all into thinking she was a healthy newborn.
For this reason, many states (37 as of today) mandate a newborn screening test called Pulse Oximetry to detect critical congenital heart defects. Pulse Oximetry is a completely painless, noninvasive test performed typically within 24 hours of baby's birth. This test provides a reading of oxygen levels in the newborns blood. If the oxygen levels come out lower than normal range that could indicate a problem and the baby would be referred to a cardiologist for follow up. This very simple test is literally saving the lives of babies born with congenital heart disease across the country! Here is one baby whose life was saved by pulse Oximetry testing. Here’s another one. And here. And here.
While many hospitals across the country are already performing this test, not everyone is. When your baby is born ask your nurse for a Pulse Oximetry test to be done. Hopefully, they are already offering the screening, if not you can educate them on the importance of screening for heart defects and share the success stories linked in this post.
Time to Vote!
We were overwhelmed by the response we got from this year's Halloween Costume Contest. Thank you to everyone who participated. All of the children in these photos were born with Hypoplastic Left Heart Syndrome. We received over 80 entries. Now it is time to vote for your favorite!
Click here to visit the album on our facebook page:
HALLOWEEN COSTUME CONTESTLook through the photos and click the Like Button under your favorite picture. You may vote on as many pictures as you want.
Simple as that! The winner of the photo contest will receive a Sisters by Heart tote bag.
Voting will end on November 10th. The winner will be announced on our facebook page on November 11th by 5pm. Feel free to share this album with your friends. Happy Voting!
2nd Annual Sisters by Heart Avon Fundraiser
The month of November is all about Giving Thanks. What a better way to give thanks than supporting a charity and getting yourself something great at the same time? We're excited to announce that, once again, Allison Haug is hosting an Avon Fundraiser in honor of her niece, Catherine Jane. Because Sisters by Heart provided so much support to Allison’s sister in the wake of her diagnosis, Allison wanted to give back and host an Avon event, with 40% of the proceeds to go to Sisters by Heart! We are so honored and grateful for Allison’s generosity.
“Catherine Jane has a smile that lights up the entire room. In her short life she's gone through more than any child should have to, and her Auntie Allison would do anything for her. However, I had no idea what to do when we first found out she had HLHS. I knew I needed to be there for my sister, Kim and my brother-in-law, Jeff. But what could I say to them? I looked for support on the internet and thank goodness Sisters by Heart answered me. They sent a care package to Kim and Jeff and linked them up with people that could truly understand what they were going through, and to give them hope that things would be ok. I know SBH helped prepare all of us for what to expect once Catherine was born and gave us all (including me!) emotional support. I don't know what we would've done without SBH!”
To learn more about Catherine Jane and her journey with HLHS visit her blog:
www.newestbender.blogspot.com
Avon has such a GREAT product selection, with everything from jewelry, to makeup, to skincare, to kids’ items and a whole lot of stuff in between - not to mention all kinds of special deals going on. So, for those of you who haven’t checked out Avon in awhile, we wanted to give you a couple of product recommendations and suggest you head on over to Allison’s site!
STACEY'S PICKS
Tiny TilliaShopping Cart Cover
A perfect way to protect your little one from germs, especially during cold/flu season!
NATURALSKIDS Bath Time Body Paint
Stacey’s girls, Emmy and Zoe, LOVE these fun bath soaps. They’re roll on in fun colors; kiddos think they’re having fun, while parents know they’re actually getting clean in the process! And the scents are yummy! And did we mention they’re only 99 cents?!? They have fun Holiday scents as well, making great stocking stuffers!
MOISTURETHERAPY Daily Skin Defense Vitamin Mini Hand Cream
Our hands take a beating with all of the hand sanitizer we use during the flu/cold season. Help sooth dry hands with this perfect "throw-in-your-purse" sized moisturizer.
JENNY'S PICKS
SKIN SO SOFT Aroma + Therapy 3-PieceCalming Collection
Escape the stress of the Holiday’s with the soothing scent of lavender that stays with you all day.
Tiny TilliaSnowman PJ
Your little one will look adorable in this Snowman PJ set by Tiny Tillia.
KATHY'S PICKS
Tiny Tillia HoodedBath Towel
Dry off your little one in style with these adorable hooded bath towels.
Sterling Silver CZHeart on Silvertone Bracelet
Perfect bracelet for any heart mom!
These are just a few of the great deals going on at Avon right now. There’s never been a better time to pamper yourself, your kids, or someone you love than now – purchase some awesome Avon products and make a donation to Sisters by Heart while you’re at it!
FOLLOW THIS LINK TO START SHOPPING!
http://ahaug.avonrepresentative.com/online_events/AFCATHERINE
Make sure you use the link posted above so that the proceeds will go to Sisters by Heart. You should see “Welcome to my Sisters By Heart online event” written in red on the top right hand of the screen. If you have any problems let us know by emailing us at info@sistersbyheart.org.
Thank you again Allison for your generous support of Sisters by Heart!
A Heartfelt Donation: Avon
I’ll be honest. I grew up with Avon. Some of my earliest memories of my mom were of her thumbing through her latest Avon catalog (dropped off by our local sweet little old Avon lady), wearing Avon’s signature Odyssey perfume. But I hadn’t thought of Avon in years…that is, until a few weeks ago, when we were contacted by Avon representative Allison Haug. Allison let us know that her niece (due any day now!) was diagnosed with HLHS this past summer. Because Sisters by Heart provided so much support to Allison’s sister in the wake of her diagnosis, Allison wanted to give back and told us she wanted to hold an Avon event, with 50% of the proceeds to go to Sisters by Heart! We were so honored and grateful for Allison’s generosity.
I was excited to check out Allison’s website, with images of my mom’s Avon in my mind. Boy was I in for a surprise when I checked out the site! Although they still had all of the classic products, they have so much more now!!! Avon has such a GREAT product selection, with everything from jewelry, to makeup, to skincare, to kids’ items and a whole lot of stuff in between, not to mention all kinds of special deals going on. So, for those of you who haven’t checked out Avon in awhile, we wanted to give you a couple of product recommendations and suggest you head on over to Allison’s site!
Avon Reversalist Renewal Cream
Amy’s pick. WOW wow wow is all I have to say. I have pretty oily skin, so finding a nighttime cream that moisturizes without breaking me out is a tall order (yes, at 36 I manage to have both acne and wrinkles all at the same time which somehow doesn’t seem fair!). But this cream absolutely does! It manages to moisturize really well, yet do so lightly. I discovered this cream thanks to Allison’s event, and I’m so grateful – it will be my go to night cream from now on!
Nathaniel the Story Time Bear
A pick for our heart babies. How cute is this little bear?!? And he recites “Twas the Night Before Christmas”? Seriously, what better Christmas present for our sweet little heart babies?
NATURALS KIDS Bath Time Body Paint
Stacey’s pick. Stacey’s girls, Emmy and Zoe, LOVE these fun bath soaps. They’re roll on in fun colors, so kiddos just think they’re having fun, while parents know they’re actually getting clean in the process! And the scents are so yummy!!! And did we mention they’re only 99cents?!? And they have fun Holiday scents as well?
These are just a few of the great deals going on at Avon right now. There’s never been a better time to pamper yourself, your kids, or someone you love than now – purchase some awesome Avon products and make a donation to Sisters by Heart while you’re at it! Just use this link and make sure that BABYBENDER shows up as the coupon code!
Thank you again Allison for your generous support of Sisters by Heart!
Practitioner's Perspective: Family Centered Care
by Michael V. DiMaria, M.D.
Children's Hospital Colorado
Family centered rounds have been introduced in many children’s hospitals for several reasons, but one of the primary motives is that families like to be involved in the health care decisions of their children. Family centered rounds are also a manifestation of a change in the culture of medicine, which has occurred relatively quickly. The way we as physicians practice medicine has shifted from what was a more paternalistic model to a cooperative one; this is addressed very explicitly in medical school curricula: we are in the era of ‘patient autonomy In pediatrics this translates into ‘family autonomy.’ The consequence of the rapid change is that both health care provider and patients can be unfamiliar with the process, and unsure of how to make best use of this opportunity.
To understand what this means for families, let’s start by talking about what to expect on morning rounds. First thing in the morning, after the incoming team of providers has gotten up to speed on developments from the overnight shift, the group gathers at each patient’s bedside in turn. The goal will be to review the events of the last day, discuss how the patient is doing, and come up with the plan for the next day. This is an important time for everyone on the medical team and the family to get on the same page. Often times, especially at a teaching hospital, a large crowd will be present. In order to make things flow more quickly and easily, the attending may ask that any questions or concerns be raised at the end of the presentation; it is difficult for the team to stay focused and efficient if there are frequent side conversations.
Next, the players: the patient’s nurse will be at the bedside, advocating for the family, bringing up unresolved issues, and clarifying his role in the plan. A resident or fellow will ‘present’ the patient to the group, meaning that she will be responsible for knowing all the details about the patient and summarizing them efficiently to the group. To briefly explain how she came to be in this position, after graduating from medical school and receiving an M.D., she did a 1 year internship, then began a 2-5 year residency; after residency, she may do an additional 3-4 years of training, called a ‘fellowship’ to sub-specialize. After finishing all of her training, a doctor becomes an ‘attending physician’ – the person in charge of the team. The attending will be listening, teaching, and guiding the trainee through the process of assembling the data and figuring out what to do next. Various other people may be present, including pharmacists, nutritionists, nursing leadership, physical therapists, etc.
As alluded to above, rounds will consist of a brief description of the day’s events, a review of the physical exam, then a bunch of numbers (lab values, fluid intake and output, ventilator settings, etc.). At the end of all of this comes the assessment and plan. It goes without saying that during the assessment the presenter verbalizes their impression of how the patient is doing. The plan is usually presented in parts, according to ‘organ systems’ (all of the respiratory issues are grouped together, as are all of the cardiovascular problems, etc). This will sound something like, “From a respiratory standpoint, I think we can try to decrease the oxygen from 2 to 0.5 liters per minute. From a nutritional standpoint, I think that Sam can try to eat a solid diet today…” This will continue until all of the active medical issues have been addressed.
When patients and care providers first encounter family centered rounds, some may find it uncomfortable to have conversations about sensitive topics in the presence of a large group. Of course, there should always be the option for the family to have a more private conversation with only the essential members of the team, should there be concerns about privacy. From the resident’s perspective, my colleagues and I were initially very nervous about presenting a patient history and physical in front of the patient’s family as a resident. Aside from being a little shy, I think I was nervous that I would get something wrong and that the family would correct me in front of the boss. I quickly got over this fear, when it became obvious that the common goal was historical accuracy.
There are several points during the process when the family’s input will be especially helpful. It goes without saying that nobody knows a child better than the primary caregivers, and so who better to be the definitive source of historical information? Because team members may come and go twice a day (at the end of a 12 hour shift), none will have the perspective of the family, who will have been with the patient continuously. Being able to give the team an idea of the overall trend of the patient’s symptoms can be very helpful. Similarly, it can be difficult for people who don’t know the child to tell what sorts of behaviors are personality-related and which are indicators that things are not quite right.
The goal of this process is to get the patient home, feeling well, and able to participate in all of the things that go into being a healthy, happy kid. More often than not, this means that the family will need to continue some interventions in the home. So, part of having a child in the hospital is learning about the disease and the treatments. Being an informed caretaker will better enable the family members to identify when problems occur at home, and what to do about them. Some measure of our success as care providers is whether or not the family feels comfortable once they are discharged. Our hope is that the shared knowledge and unified goals of families and care providers results in a close working relationship that develops in this setting of family centered care.
Possibilities: Cord Blood Banking
With the recent flurry of stem cell research associated with HLHS infants, Sisters by Heart wanted to make certain our expecting families were aware of an important opportunity through Cord Blood Registry® (CBR®).
CBR offers the Newborn Possibilities Program which provides families, with an identified medical need, free cord blood processing and storage for five years. Because of the potential of newborn stem cells as a treatment for HLHS, CBR is accepting applications from families expecting a baby with a prenatal diagnosis of HLHS for inclusion in their program. Applications are reviewed and accepted on a case-by-case basis. CBR encourages all expecting HLHS families to apply. The ultimate benefit, if successful, would be treatment for HLHS… if your application is accepted: FREE banking and storage for five years.
"I had always thought about saving my baby’s stem cells but never had the funds to do so, that's why I am so excited about this program. The application is extremely simple, consisting of some personal information, a doctor's signature, and medical file to confirm the HLHS diagnosis."
~ Kristina Marsh, Expecting HLHS Momma.
We've asked another of our expecting moms to share her experience in applying for the Newborn Possibilities Program.
“Thank God for Sisters By Heart. At 19 weeks we were diagnosed with HLHS for our little "Peanut." I immediately turned to the internet and looked for others out there that had lived that horrifying day when I felt the world crumble. There they were, my Sisters that I have never had. One particular “sister” got stuck with me because of where we live, and THANK YOU GOD FOR HER. Natasha Saywer heard my cry for help and responded to me immediately. She put herself out there and came to meet me with her little heart baby, Evan. It was one of the greatest days of my life. My hope for help became a reality for me.
As I sat with Natasha over breakfast, drilling her with questions, I fell in love with her HLHSer, Evan. He's my hero. We discussed so many things, including cord blood banking. Natasha mentioned the potential for free banking through CBR. I looked onto the idea and ran with the information she'd provided me.
Three days after meeting Natasha for breakfast, I called CBR and inquired about such a program. A CBR representative informed me about the Newborn Possibilities Program. She described it as an easy, free process. I provided my email address and she emailed me everything that I needed. I filled out a short application and sent one page to my OBGYN for completion. Within a few days, I faxed the forms back to CBR.
A week after applying for the program, I received a phone call from my CBR representative. She told me that CBR's Medical Board approved my application for free banking and five years of storage, free of charge! I was ecstatic! After the first five years, we will need to begin paying $130 annual storage fee if we want to keep our baby’s cord blood stored for future use. But, the initial banking and first five years free is an INCREDIBLE savings.
Easy and Painless.... Thank you so much again Sisters By Heart and Natasha Sawyer for guiding me. Thank you so much Cord Blood Registry for accepting our application! I know Sisters By Heart does a lot behind the scenes and myself, my boyfriend and "peanut' are so thankful for everything you do not only for us but for everyone. We love you all’.
Leigh-Anne Dowdle
If you want to learn more about CBR’s Newborn Possibilities Program, please email us at info@sistersbyheart.org or visit cordblood.com.
A Unique Partnership
Sisters by Heart and the National Pediatric Quality Improvement Collaborative (NPC-QIC) are teaming up to improve care for HLHS children and encouraging data sharing amongst cardiac centers. We need your help!
Please take a few minutes of your time to fill out this survey. We'd love to have hundreds of parent responses; all parents of children with Hypoplastic Left Heart Syndrome are invited to complete the survey.
The survey will remain available until Friday, September 13, 2013. Your participation is greatly appreciated! https://www.surveymonkey.com/s/NPCQIC_SByH_ParentSurvey
Fontan Series: Lily's Story
The Fontan: Our Story
Hi my name is Julia. Our daughter Lily is 7 years old and has Hypoplastic Left Heart Syndrome (HLHS) and a pacemaker. She has completed the three-staged surgical repair and is growing and doing very well! We are a CHOP family, and you may have seen Lily’s face on billboards and print material in the Philadelphia area.
I was asked by Sisters by Heart to share our Fontan story with the group. I am always happy to give support and guidance to families who are in the midst of that extremely long wait inter-stage. I remember feeling like we were in a “holding pattern” for quite some time!
When I was approached to share our experience, I made SBH aware that it would not be one of a lot of sleepless nights or feelings of being totally overwhelmed. I don’t want to minimize the impact of having a child with complex CHD on one’s physical and emotional health, but to me the Fontan was just the next step that had to take place for our daughter to move on with her life. You see, I refuse to let the terms CHD or HLHS define who Lily is as a child, or who she will become as an adult. Granted, we never asked to be given a sick baby, but that was the card we were dealt. Some people say that “everything happens for a reason.” I’m still not so sure how I feel about that statement, but I do know that sometimes things happen differently then we planned.
Sometime between the initial diagnosis, and Lily being born I made the decision that I was going to do everything in my power to give Lily a life that was as “normal” as possible, no matter what it took. We all have different ways of seeing what is best for our child, and I in no means try to push my feelings onto others. I completely understand the anxiety and feelings of depression that come along with having a sick baby. I feel blessed that we had a cardiologist who wasn’t overly conservative and always told us to let Lily live life and have new experiences even with an HLHS diagnosis.
In 2009 at 3.5 years of age Lily was admitted to CHOP for her Fontan. My husband and I decided not to tell her that we were going to the hospital until a few days before the surgery as to not worry her. In Lily’s case, she tends to be a worrier, and we felt that telling her too soon would cause much undue anxiety and stress. We were first case that day, and Dr. Spray performed the Fontan surgery which only took about one hour total to complete. Lily was taken to the CICU immediately after surgery, and we were able to meet with Dr. Spray who said the surgery went very smoothly with no unexpected complications. (Thank god!) Lily had an extracardiac Fontan with a fenestration.
After our meeting with Dr. Spray, we were able to return to the CICU to see Lily. Her chest tube was removed later that evening, and by the next morning the nurses had her sitting up and taking her first steps around the room. Lily was fortunate in that she did not develop the pleural effusions that can sometimes be associated with the Fontan repair. Lily had her surgery on Friday July 9th, and was discharged home on Monday morning July 12th after a 3 day stay. Here is a picture that was taken the day of her Fontan.
It has been almost 4 years since that date, and Lily has been doing so well. She is in the first grade at our local public school, and is very smart. She requires no special accommodations in the classroom or during school activities such as physical education class. We do have a Medical Plan set-up with her school that the nurse and all teachers are aware of and follow, and I keep in regular communication with the school administration and faculty. Lily is also very active and participates in many sports including softball, gymnastics, and dance. She loves arts and crafts, swimming, and riding the roller coaster at Sesame Place during the summer.
So I guess what you can all see is that Lily is a pretty cool kid! Do I always have in the back of my mind that she is a heart kid? “YES!” Do I wonder on a regular basis whether she will someday need a transplant? “YES!” Do I worry what her life will be like when she is 30 and whether she will be able to have her own children? “YES!” But will I let these fears and uncertainties hold us or Lily back?? The answer is “NO.” And the answer is no for one reason, and that is because I choose not to. We are only given one life, and I want my daughter to have a life that is filled with wonderful, positive memories. I want her to not define herself as a “heart kid”, but as a kid with amazing heart!!
Julia Rowbotham, Lily’s Mom
Thank you Julia, for sharing Lily's story and allowing us to share in her inspiring journey!
Preparing Your Child for the Fontan
By: Sherry Polise, CCLS, Child Life Specialist III - The Cardiac Center
The Children’s Hospital of Philadelphia
“Helping Your Child Prepare for their Fontan Surgery”
The Fontan Surgery is stressful and overwhelming for parents for many reasons, but one of the most difficult aspects is because of your child’s age. Most children entering into this procedure are between 2 and 5 years old so they are just beginning to understand their body and how it works, but they are also extremely limited in the amount of complex information they can process. Parents often feel overwhelmed at the thought of talking to their 3-year-old about open heart surgery when they themselves get confused and worried when thinking about the topic. For these kids there are still plenty of things you can do before surgery that can help your child feel comfortable, have a better understanding of what is happening, and help set the stage for the most positive experience possible while at the hospital.
Before surgery, there are many things you can do to help support your child’s understanding of what is to come.
-Be honest and talk about what’s happening: First and foremost, it is important to be honest - even with young children - about what is happening while using age-appropriate language. A simple way of explaining heart surgery to a child even as young as 2 or 3 might be “remember when we went to the doctor and took the special pictures of your heart? He saw a little boo-boo that needs be fixed and that’s called surgery”. There are some 3 year olds who might hear that and ask a ton of questions right away and some who might look puzzled and immediately want to go back to playing. This range of reactions is okay and normal; the most important thing is that you are using consistent, honest, and age-appropriate language so that your child feels empowered to ask questions if they have them.
-Use simple concrete language: Kids at this age can have wild imaginations; sometimes that imagination can help them have a lot of fun, but it can also make them envision really scary things too. When taking about the hospital, try to avoid analogies and metaphors like “having a zipper” or “fixing your engine” as these can evoke confusing and scary imagery for young children. Using familiar terms like “boo-boo” or “owie” helps your child understand what you are talking about without letting their imaginations run wild.
-Be aware of timing: One common question that parents often ask is “when is the right time to tell my child about surgery?” For most children in this age range, we recommend telling them no more than 1 to 3 days prior to the procedure. This allows time for them to ask questions and process the information but not too much time to sit and worry about it or even forget the information completely.
-Ask to speak with a child life specialist: All pediatric hospitals employ child life specialists who are trained to help explain medical procedures to children of all ages. You can ask to speak to one about how best to meet your child’s needs. Often a child life specialist can use a doll or book to help prepare your child for the hospital and the things they will see on their body after surgery. Often times, they can arrange a pre-op tour with you and your child to give them an opportunity to see the hospital and ask any questions beforehand.
-Focus on some of the positive aspects of the hospital: It is important to tell your child the truth about things that are happening but make sure you emphasize the positive and the things that are important to them. Remind that them you will be with them at the hospital and that there are toys, books, and movies at the hospital too. Most children’s hospitals have a playroom as well. These things are comforting and reassuring to young children.
-Read and engage: Another thing you can do prior to surgery and just in general is to incorporate story books about the hospital or going to the doctor into your normal reading routine. Reading about your child’s favorite character going for a check-up or visiting the hospital can help normalize these things for them and provide an opportunity for dialogue about these experiences.
-Use medical play: For children at this age, they are also learning about and processing their world through play. Medical play can be extremely helpful for children in giving them an opportunity to “be the doctor” instead of the patient. You can help your child by providing them a play doctor’s kit and a doll and simply being there as a reflective listener during the play. You can also listen to your child while they are being the doctor and clear up any misconceptions you overhear.
-Help them to take charge: You can also help your child prepare for surgery by helping them have some control over the situation. As you well know as the parent of a preschooler, a sense of independence and control is very important for them. You can foster that sense of independence by allowing your child to help pack their bag for the hospital and allowing them to include the things that are important to them (i.e. a favorite DVD, favorite sippy cup, pajamas, etc.). Siblings can help too!
-It is okay to not know: If your child asks you something about the hospital that you don’t know or aren’t sure how to answer in a way that isn’t too scary, you can be honest and say “that’s a great question, I’m not sure but let’s write it down and we can ask when we go to the hospital”. This can give you an opportunity to think about your response but also assures your child that you will get them the answer.
You can also find more information and helpful tips on preparing your child for surgery here.
Thank you Sherry for sharing your insights and advice on preparing for the Fontan! We are truly grateful for your expertise.
Fontan Series: Aly's Story
When I started thinking about writing a post about the Fontan, there was one thing that really made me smile. I really had to sit down and think pretty hard to remember back to our daughter's Fontan and it was only two years ago. Over the last two years since our daughter, Aly, had her Fontan surgery, life has really taken a turn - a big huge turn towards NORMAL. We are living a life now that we dreamed of and honestly, weren't sure was attainable when we found out about her special heart. But now looking back, here is my reflection on the Fontan.
In hindsight, the anticipation for the Fontan was worse than the actual Fontan. I was a mess during the last few months leading up to the Fontan - worried about everything under the sun. Could we do this again? Could she handle this? How would it be with an almost two year old? What do we need to bring? Will she forgive us? Will she remember? What kind of clothes should we bring? What about shoes? What about sippy cups and her favorite snacks? I could go on and on and on... Here are the answers to these questions that I learned.
On the way to the hospital for our daughter's Fontan, I had a little breakdown where I begged my husband to turn around and go home. I was looking at my sweet girl who hadn't been in the hospital since she was discharged from her Hemi-Fontan at four months old. She had been living a typical baby life for 18 months and now we were forcing her down this road again. My husband reminded me that this was a decision we made long ago - to fight for our girl - and there was no turning back. All of this I, of course, knew but I needed to be reminded. So we kept on our way with our car packed to the ceiling with what I anticipated to be our every need for the next 7-10 days. (That was the average hospital stay for the Fontan that they had provided us with for planning reasons. Over the last few years I have noticed that this is pretty typical- of course, there are longer stays and there are shorter but on average I think 7-10 days is pretty accurate. You know, from my completely non-medically trained heart mom opinion :)
In pre-op on the day of her Fontan
Our daughter's Fontan went very smooth from "go". We were first case for the day so we got to the hospital early. Aly had a hefty dose of Versed and she was off to the O.R. 4 hours later, we were by her side in the PCTU. She was so PINK! She was extubated within an hour of settling in to her room and, as her Cardiologist put it, sailed through her Fontan.
A few hours post-op, on only a "whiff" of blow-by oxygen.
By day 4, we were told that clinically she would be ready to be discharged but she was having some excessive draining in her two pigtail tubes. So we spent the next four days just waiting for the drainage to subside. Aly really did amazing.
Day 6 post op, sitting in our hotel room (in the hospital) having a snack. You can see her drain tubes coming out from under her shirt.
She did have anxiety issues whenever doctors, nurses, volunteers, etc, came around but the hospital was really great working with us. They would do rounds outside of her door instead of around her bed and come in to see her one at a time. The nurses let us do her vital checks while they waited on the other side of the curtain. By day 6, we were off all monitors and had free reign of the hospital. We had to check in once for every 8 hour shift for vitals checks but that was it. Finally, on day 7, Aly had the last of her drainage tubes removed; we stayed one more night to be sure there would be no fluid accumulation after the tubes were removed and we were OUTTA THERE! Literally, simple as that.
Day 8 - DISCHARGE DAY! On our way home. :)
Emotionally, Aly did so well. She recovered well and doesn't seem to have too many memories of her Fontan. She remembers sleeping in the hospital and us being with her. She remembers watching movies and eating cheeseburgers in bed.
The biggest stressor in the Fontan planning process for me... "How was I going to keep a toddler entertained while in the hospital?" I had bags and bags and boxes of toys. My hope was to have a grab bag of sorts so that anytime she was having a hard time, I would have a new toy for her to play with. She was OBSESSED with singing cards at the time so I had gotten her a new one to open everyday. I bought all new sippy cups and every snack I could think of. In hindsight, I went a little overboard. :) I hadn't really taken into consideration that she wasn't going to be feeling 100%. The way she felt during recovery I would compare to how she acts when she has the flu at home. She just wanted to snuggle, cuddle and watch movies. We should have brought more snuggly blankets, pillows and movies and a few less toys. I am glad we brought the sippy cups and the snacks. Getting her to eat and drink after surgery was a little challenging but it was made a little easier that we had her familiar cups that she was used to and snacks that she loved. And it didn't hurt that she could eat cheeseburgers and tator tots for every meal if she wanted since those were her favorite. Nobody cared what she ate, as long as she was eating.
Another part of planning that I would have done differently is to bring more nightgowns and dresses (simple over the head outfits). It seems with most Fontan patients, if their stay is prolonged it is because of the darn drainage so you will be battling tubes when attempting clothes so things that slip on and off easily over the head were best for us. Aly spent most of her time sporting t-shirts and leg warmers. :)
Every hospital is different with their post-op guidelines. Some require post-Fontaners to get up walking ASAP and some aren't as adamant. Some insist on a fat-free diet and fluid intake restrictions and others don't. As with every other step of this journey, there is no standard that all hospitals follow. My advice would be to discuss this beforehand so you will all be on the same page as for what to expect post-op.
I know the Fontan is a scary thing to prepare for but we pictured it as a finish line. We know that there will be more ahead for our girl down the road but nothing we can anticipate or plan for as we had been anticipating the three staged surgeries. Looking back, for Aly it was the easiest recovery of all of the surgeries. There was no "Hemi- head" headaches to deal with or any of the struggles of Norwood recovery.
This is one of my favorite pictures of Aly. This was her 10 days after her Fontan. Playing outside like nothing every happened.
A Heartfelt Donation: Medical Masks in Anya's Memory
Many of our families appreciate most, our care packages which are specially designed for newly diagnosed HLHS families. We're always humbled when families contribute to our care packages in honor and memory of their children.
Today, we wanted to share a mom and daughter whom we hold close to our hearts. What better way to honor her motherly instinct than helping other moms do the same.
Karen and Anya Wockenfuss
I'm Karen Wockenfuss, and I consider myself blessed to be a heart mom. I found out at 19 weeks pregnant that my precious baby girl Anya had Hypoplastic Left Heart Syndrome. A parent never forgets those words "your baby has a congenital heart defect." She was born at 3:24 AM on August 27, 2012 weighing 6lbs 2oz. She had her Norwood procedure at two days old, and although the surgery went well she had a few complications afterwards (chylothorax and blood clots requiring lovenox injections). She also needed a feeding tube and had g-tube surgery at 6 weeks old. She finally came home on October 16, 2012, at 7 weeks old. Having her home was the best 15 days of my life, and I loved my new normal. I am a heart mom.
Karen's precious daughter, Anya
Anya suddenly passed away on November 3, 2012, for reasons unknown. I miss her so much. In becoming a heart mom I have met so many amazing, strong people, in those heart warriors still fighting and their parents. I am passionate about staying involved in the CHD community and keeping Anya's memory alive.
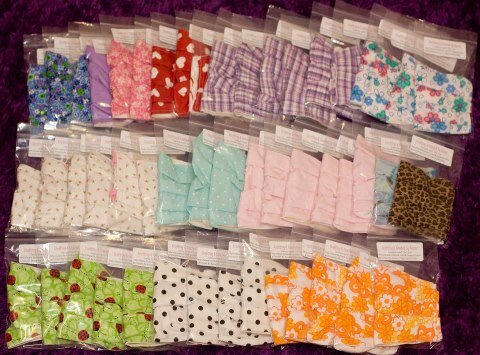
I make re-usable, machine washable face masks for adults and kids in cute prints. In Anya's memory, I am donating 50 of my adult face masks to Sisters By Heart to be included in their care packages. These will be especially useful for moms right after their baby has had the Norwood procedure. In addition to the initial 50, for every face mask I sell, I am also donating an additional one to Sisters By Heart.
To order your own face mask for $8 (or 2 for $15), please visit 'Crafting & Crochet by Karen' on Facebook: http://www.facebook.com/pages/Crafting-Crochet-By-Karen/172687209455948
To read the rest of Anya's story, please visit: http://emoreeandme.blogspot.com
Thank you, Karen, for thinking of our families in your time of grief. We know our families will truly appreciate this gift from your heart. Karen has been busy and has already shipped 100 masks to Sisters by Heart for inclusion in our care packages!
They're such a perfect addition to our packages, as we always love to promote health and happiness during the interstage period!
Karen's generous donation in memory of Anya
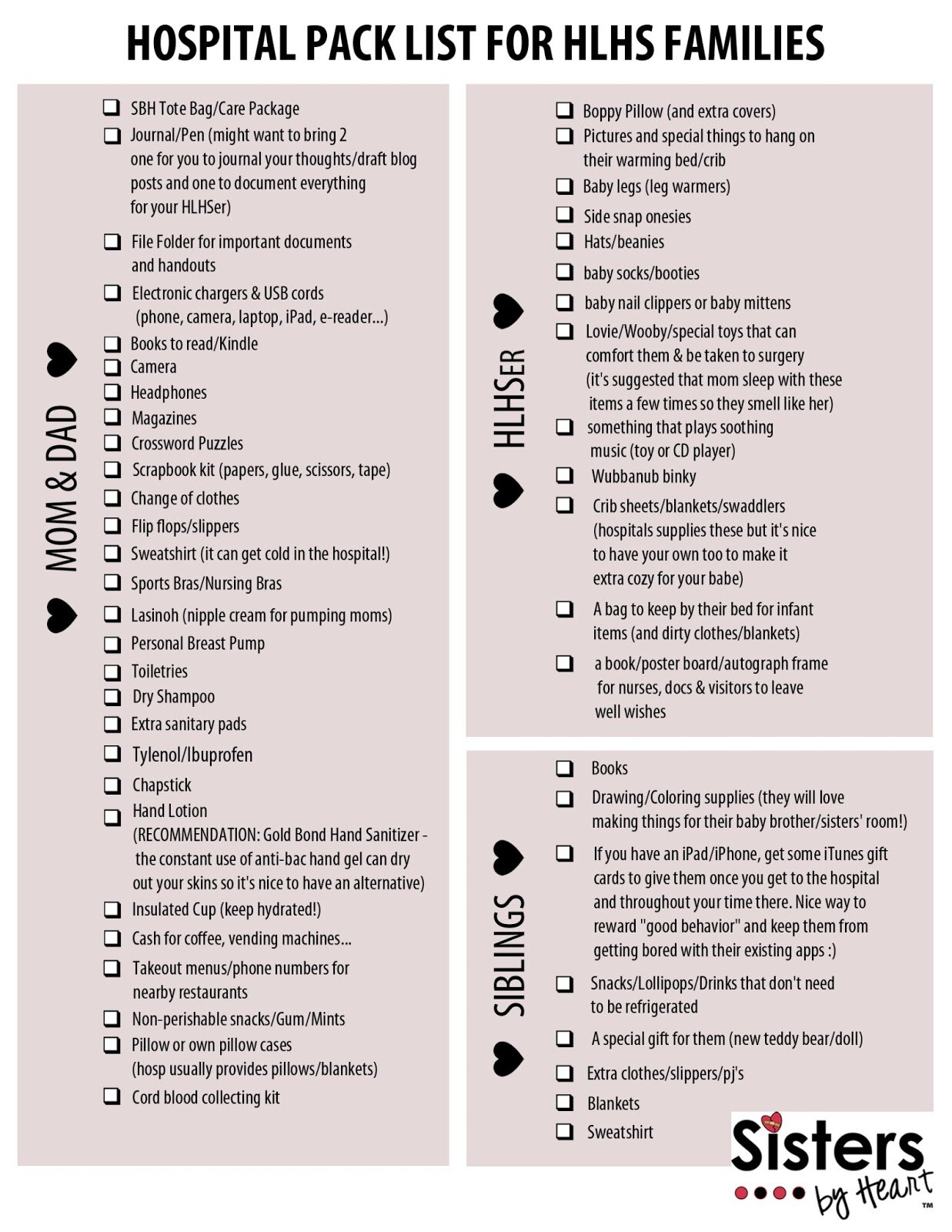
Parent's Perspective: What to Pack for the Hospital
One of the most-asked questions by our expecting moms is, "What should I pack for the hospital?!"
In response, we reached out to our experts, the heart parent community, to ask what they found helpful. We've collected their suggestions and created the below checklist in an effort to make packing much less stressful! While the list is geared more towards expecting families, it's really great for anyone facing a hospital stay with their child. The list contains suggested items for baby, parents, siblings and a 2nd page for relocating families. It's in a printable format so you can right-click-save and print a copy when you are ready to start packing!
If there are any items items you found helpful that we have not listed, please let us know and we will keep the list growing!
Happy Packing!
Getting a 2nd Opinion: An Inpatient Perspective
Earlier this week, we shared the story of a family who sought a second opinion for their son while he was outpatient and non-critical. Today, we bring the story of a family who sought a second opinion under completely different circumstances, for their son, who was inpatient and very critical. Thank you, Teri, for sharing Finley's story!
(Teri and Finley)
Hopefully this subject never pertains to your child, but if it does, I hope this post will help you navigate the process easier.
Requesting a second opinion does not mean that you have lost faith in your home hospital and team. Since larger hospitals have a higher volume of patients, they have seen and dealt with more complications and may have ideas your home hospital is unaware of that could help resolve the issue. Unfortunately, our situation was such that we wanted a transfer, not just a second opinion. It is up to you to decide which avenue you wish to seek. Sometimes the second opinion you receive will propose a plan that your home hospital cannot perform and a transfer would be required to implement the plan.
A little background – My name is Teri Chrislip. My son, Finley, is 23 months old and is 13 months post Glenn. He was discharged five days post surgery on a low fat diet with a blake drain due to chylous effusions. They told us that it could take up to six weeks for it to resolve. His surgeon felt we were capable of managing his care at home during this time. We had no idea it would turn into a six month nightmare. Finley was in and out of the hospital multiple times due to electrolyte issues caused by the drainage. Those stays included two caths, one of which turned into an emergency open heart surgery. We finally came to the realization after rushing him to the emergency room with labored breathing which led to another PICU admission that we needed more input. We made a verbal request of our team that day to send his records off to Boston to get a second opinion. He was averaging 30 ounces of drainage a day. Six days later, Finley coded and we made the decision that a second opinion was not enough. We wanted a transfer.
My inner mama bear went in overdrive. I contacted another heart mom to help us seek our own second opinion from Boston because we were not having luck working with our home team. She put us in direct contact via email with Dr. Jim Lock, the head of cardiology in Boston. Thankfully, upon reviewing his file, Dr. Lock felt he could help Finley and wanted him transferred to Boston so he could perform a life saving cath. Because his plan could not be implemented at our home hospital, Finley’s air medical transfer was approved in three days. Dr. Lock performed his cath four days after our arrival in Boston. Within eight weeks of that cath his drains were removed and we have been home for over seven months straight! We are still weaning diuretics, but Finley is doing amazing. He has gained over six pounds and is making huge strides in his development.
Below are the steps I suggest for any parent seeking a second opinion and/or transfer when your child is in critical condition:
1. Pick the hospital you want to seek a second opinion from and contact them directly yourself. If seeking a transfer, I would narrow it down to one hospital. In my opinion, if you do not narrow it down, you could get two different opinions that could hold up the transfer process. If requesting a second opinion only, you could request opinions from several hospitals. Each hospital is a little different on how they handle second opinions and/or transfers. Advise them that you have a critically-ill inpatient child and your needs are very urgent. They will provide you the requirements on what information they need to prepare a second opinion and where to have it sent. Most hospitals will request your most recent echo and cath (on disc) along with recent surgical and inpatient reports. If you do not already have a cardiologist and surgeon in mind, they will likely assign one for this process if it is required. Our home hospital would not send files without them being directed to a specific doctor(s). If you are unsure on who to contact or how, ask your fellow heart moms. Most top hospitals have a dedicated phone number or email address specifically for second opinions. Scour their website; I know Boston has each physician’s email addresses listed.
2. Once you know what you need and where to have it sent, put your request in writing to your current team. This was one of our biggest mistakes. We lost an entire week by starting with a verbal request that was not followed through on. Be sure to include a deadline of when you expect them to have the files sent. We gave them 24 hours due to the extreme critical situation. Just prepare yourself that it could get confrontational. If only asking for a second opinion, some doctors may take it personally. If asking for a transfer, some doctors and hospitals will be worried about being accused of negligence. They may be scared that the new team could find errors they made, simple things they missed, etc. As soon as we notified them of our intentions to transfer, we had more doctors involved in Finley’s care than we had the whole time! The attending cardio had not been in to see Finley for the entire week prior to our request. Trust me, no hospital wants a lawsuit on their hands!
3. Contact your insurance company immediately to see what their requirements are for a transfer. They are pretty hard to get approved, especially air medical transfers. We had a wonderful nurse case manager that helped us facilitate our request. The biggest issue in getting a transfer approved is that the receiving hospital must be proposing a plan that your home hospital cannot implement, and your home hospital must admit that to your insurance company. If not, most insurance companies will not agree to a transfer, suggesting instead that your home hospital implement the plan laid out in the second opinion. If so, you can appeal that your home hospital is not as capable as the proposing hospital and the outcome would not be as favorable which would cause a longer hospital stay. We voiced our unhappiness with our home hospital and the poor care he had received. Also, he had already had several surgeries and lengthy, expensive stays with no results. So in the end, I am sure they justified that the costs to transfer him to a hospital that could hopefully resolve his issue was far less expensive than to continue the path we were already following at our home hospital. As we all know, the insurance company will weigh the costs versus outcome. Your other option is to pay for the transfer yourself, but it is very expensive. Our air medical transfer one way was $36,000 with insurance negotiating the rate to $18,000. You could also check into Angel Flights or other organizations that help with medical transfers. Typically one parent can fly with the child. I flew with Finley and our social worker at our home hospital provided us a prepaid round trip commercial flight for my husband.
4. If transferring, contact the social workers at the hospital where you are transferring about parent lodging and other services available. In Boston, only one parent can sleep in the room with the patient. Since we both were there, we had to make lodging arrangements. We were provided with a sleep room while he was in the CICU. Once he was moved to the floor we had to find other arrangements. Each hospital has different parent lodging available, so check with the social worker on your options. Also, your meals will begin to add up. Be sure to check to see if there is a meal voucher program, especially if you are breastfeeding. It may be only a few dollars a day, but depending on the length of your stay it could be a big help.
Remember, if you are ever in the unfortunate situation of needing a second opinion and/or transfer it is not your fault. Do not be afraid to ask for and accept help from as many people and organizations as you can. Even though we had traveled to Boston for vacation previously it was still scary. We knew the ins and outs of our home hospital and lived only 30 minutes away. Taking a medical flight half away across the country and having our child admitted to a new hospital was overwhelming at first. Just remember, you have been through a lot already and you can do this for your child. Just put one foot in front of the other, one step at a time!
Getting a 2nd Opinion: An Outpatient Perspective
We often hear heart moms asking whether or not they should seek a second opinion. Our response is always the same – even if your child is not critical, if you have any concerns about your child's care, yes, you should definitely seek out a second opinion. With complex CHDers, a second set of eyes never hurts.
In the next two blogposts, we’ll be sharing the stories of two families who sought second opinions for their HLHS children. First is Paxton and his mom, Jessica, who sought an outpatient second opinion leading her across the country for Pax’s Fontan surgery. Jessica shared with us some great insights about what the second opinion process is like when your child is outpatient and not-critical, and how to go about maintaining good relationships with your home care team during the transition.
Thank you, Jessica, for sharing your journey with us!
Jessica and Paxton
Almost six months ago I passed my three-year old son over to a surgical team for his lateral tunnel Fontan at Boston Children’s Hospital. What had started as an information-gathering opinion on my son’s complicated heart and pulmonary structure turned into a 1,800-mile trip from home to the team who has ultimately saved my son's own heart.
A few months prior, I sat listening in disbelief as our “home” cardiologist sprung it on me once again that we were possibly headed down the road of heart transplantation. It had been discussed off and on since Paxton was five days old. Despite having had a dozen heart procedures, many being emergencies, Paxton was thriving with half his heart and a compromised left lung. I asked myself, “How could a child doing so well need a new heart?”
That very day I felt a strong urge in my heart to seek another opinion. I knew I had one chance at my son’s life. It was so hard to tell the team who had saved my son’s life time and time again that I needed more. After all, they became part of our extended family. I apologized repeatedly, but his cardiologist reminded me that Paxton was his baby too, and that he also wanted the very best for him.
Were his feelings a little hurt? Yes. Was his pride a little less? Yes. Did he shed a tear or two as we were leaving? Yes. I truly think it was because he had been working to save Paxton for years. He knew his case well and the thought of someone new inside my son’s chest concerned him. Upon my request, every detail of Paxton’s history was sent to Boston Children’s Hospital for a second opinion.
A top cardiologist at Boston Children’s was selected to review Paxton’s extensive and complicated history. A few weeks later we received the report in the mail that concluded Paxton had received good care at his home hospital and that they would have done nothing differently with his treatment at Boston. That was so reassuring to me because I was not seeking a second opinion to find fault. We did and always will love our home team. But what came next in the report stirred my emotions as a mother of a fragile child whom we had fought so hard to save. A final recommendation of treatment could not be made unless Boston performed a heart cath on Paxton. The report gave me no clear answers. Did my son truly need a new heart? And would my son with a compromised left lung even be eligible for a heart? My heart ached for more answers from one of the very top heart teams in the country. I knew we had to make the trip from Missouri to Boston.
I was at peace the very moment my eyes looked at Boston Children’s Hospital. A sign ran across the entrance to the building that read “Ranked #1 – U.S. News & World Report.” At that moment I realized just how easy and worthwhile the process had been to get a second opinion. What once was just a dream of having my son treated at a top heart center had turned into reality. My fears of getting lost in the crowd at a large heart center were quickly erased. I felt as if my son was their only patient. I felt as if they loved my son even though they had just met him.
As hard as it is for me to admit, there is a difference between good heart centers and the BEST heart centers. The best heart centers have the collective experience to tackle the high-risk cases and are the ones researching new treatment plans that trickle down to smaller heart centers, like our home hospital.
After completing every heart test available, Paxton went in for his pre-Fontan cath. One of the very best interventional cardiologists in the world performed the procedure and advised us that Paxton was a candidate for the Fontan. It would be considered higher than average risk, but she believed it could be done. She advised against heart transplantation.
Paxton had been at risk of sudden catastrophic event since birth. Every procedure up to this point had been high risk when it came to our son. We were not afraid to proceed. The next decision was whether or not to have the surgery performed in Boston.
The fact that my son would have a Fontan to one and a half lungs made the decision to go to Boston easy. At Boston, a team of 75 of the best heart doctors in the world would be surrounding our son, discussing his complex anatomy.
Simply put, Boston offered us more hope and experience. I chose Boston not because our home team was not really good, but rather because for this period in time Paxton’s heart required the very best!
The senior surgeon hand-picked for Paxton’s set of circumstances is in the top 1 percent in his field. He is confident and this brought me so much comfort. Even though I felt uneasy about the unknowns of traveling across the country for a risky surgery that could require a timely hospital stay, I felt such peace in the decision I had made.
Paxton amazed everyone in that he sailed through the Fontan surgery. He was up walking around the CICU with tubes coming out of his body the second day after his surgery. Paxton was back home in Missouri in just one week. Our home team could not believe that Paxton walked through the doors to see them for his post-Fontan check up just one week after boarding a plane for Boston.
All the emotions that our team back home might have felt about seeing him go to Boston all went away after they looked at him. They knew we had made the right decision for our son and they showed so much pride in our success.
Paxton’s home team is still his team. We will never take that away from them. They still love him and are still involved in his care. They are ultimately the ones who gave him his chance at life the first 12 times. It is just that we have now added to our team of lifesavers. Boston Children’s ultimately saved my son’s heart when our home hospital was considering giving up on it.
A recent post-Fontan check up at Boston Children’s proved that Paxton’s very own heart is the best that it can be. We will continue to have them check on Paxton for the years to come simply because they are one of a few heart centers, such as the Children’s Hospital of Philadelphia, that are thinking outside of the box for the future of our HLHS kids.
My husband and I are fortunate to have exceptional health insurance that paid for Paxton’s treatment in Boston. I understand that not every family has the same resources. The second opinion itself was provided at no cost by Boston Children’s Hospital. The same is available for all heart children.
I find comfort and rest knowing that I followed my instinct to get a second opinion and to follow where my heart led my son. I also find comfort in his home team that we still trust for his day-to-day care.
Ultimately, I am my son’s advocate. It is not about sparing feelings and it is nothing personal to seek another opinion. I would do it all over again. Sometimes it is necessary to separate ourselves from the team we love to make sure we are giving our children their best chance at life.
Preparing Your Child for the Fontan
Sherry Polise, CCLS
Child Life Specialist III
The Cardiac Center
The Children’s Hospital of Philadelphia
Helping Your Child Prepare for their Fontan Surgery
The Fontan Surgery is stressful and overwhelming for parents for many reasons, but one of the most difficult aspects is because of your child’s age. Most children entering into this procedure are between 2 and 5 years old so they are just beginning to understand their body and how it works, but they are also extremely limited in the amount of complex information they can process. Parents often feel overwhelmed at the thought of talking to their 3-year-old about open heart surgery when they themselves get confused and worried when thinking about the topic. For these kids there are still plenty of things you can do before surgery that can help your child feel comfortable, have a better understanding of what is happening, and help set the stage for the most positive experience possible while at the hospital.
Before surgery, there are many things you can do to help support your child’s understanding of what is to come.
Be honest and talk about what’s happening: First and foremost, it is important to be honest - even with young children - about what is happening while using age-appropriate language. A simple way of explaining heart surgery to a child even as young as 2 or 3 might be “remember when we went to the doctor and took the special pictures of your heart? He saw a little boo-boo that needs be fixed and that’s called surgery”. There are some 3 year olds who might hear that and ask a ton of questions right away and some who might look puzzled and immediately want to go back to playing. This range of reactions is okay and normal; the most important thing is that you are using consistent, honest, and age-appropriate language so that your child feels empowered to ask questions if they have them.
Use simple concrete language: Kids at this age can have wild imaginations; sometimes that imagination can help them have a lot of fun, but it can also make them envision really scary things too. When taking about the hospital, try to avoid analogies and metaphors like “having a zipper” or “fixing your engine” as these can evoke confusing and scary imagery for young children. Using familiar terms like “boo-boo” or “owie” helps your child understand what you are talking about without letting their imaginations run wild.
Be aware of timing: One common question that parents often ask is “when is the right time to tell my child about surgery?” For most children in this age range, we recommend telling them no more than 1 to 3 days prior to the procedure. This allows time for them to ask questions and process the information but not too much time to sit and worry about it or even forget the information completely.
Ask to speak with a child life specialist: All pediatric hospitals employ child life specialists who are trained to help explain medical procedures to children of all ages. You can ask to speak to one about how best to meet your child’s needs. Often a child life specialist can use a doll or book to help prepare your child for the hospital and the things they will see on their body after surgery. Often times, they can arrange a pre-op tour with you and your child to give them an opportunity to see the hospital and ask any questions beforehand.
Focus on some of the positive aspects of the hospital: It is important to tell your child the truth about things that are happening but make sure you emphasize the positive and the things that are important to them. Remind that them you will be with them at the hospital and that there are toys, books, and movies at the hospital too. Most children’s hospitals have a playroom as well. These things are comforting and reassuring to young children.
Read and engage: Another thing you can do prior to surgery and just in general is to incorporate story books about the hospital or going to the doctor into your normal reading routine. Reading about your child’s favorite character going for a check-up or visiting the hospital can help normalize these things for them and provide an opportunity for dialogue about these experiences.
Use medical play: For children at this age, they are also learning about and processing their world through play. Medical play can be extremely helpful for children in giving them an opportunity to “be the doctor” instead of the patient. You can help your child by providing them a play doctor’s kit and a doll and simply being there as a reflective listener during the play. You can also listen to your child while they are being the doctor and clear up any misconceptions you overhear.
Help them to take charge: You can also help your child prepare for surgery by helping them have some control over the situation. As you well know as the parent of a preschooler, a sense of independence and control is very important for them. You can foster that sense of independence by allowing your child to help pack their bag for the hospital and allowing them to include the things that are important to them (i.e. a favorite DVD, favorite sippy cup, pajamas, etc.). Siblings can help too!
It is okay to not know: If your child asks you something about the hospital that you don’t know or aren’t sure how to answer in a way that isn’t too scary, you can be honest and say “that’s a great question, I’m not sure but let’s write it down and we can ask when we go to the hospital”. This can give you an opportunity to think about your response but also assures your child that you will get them the answer.
Thank you Sherry for sharing your insights and advice on preparing for the Fontan! We are truly grateful for your expertise.
Practitioner's Perspective: Pain Management and Withdrawal
By: Dr. Moffett, Pharm.D. , Texas Children's Hospital
If you've been indoctrinated into the Congenital Heart Defect community, one important lesson learned is that all CHD babies and children are different. As pediatric cardiac surgeon, Dr. Redmond Burke stated, "The babies' hearts are like snowflakes, they are never the same."
One size definitely does not fit all. A particular surgery may be ideal for one HLHS infant, but not for another. The same can be said about medication administration and pain management.
The vast majority of HLHS infants and children undergoing palliation require opiate pain medications (i.e. Fentanyl, Morphine, etc.) following the immediate post-operative period. For various reasons, pain medications may be prolonged causing an infant to become opiate dependent or "hooked."
It is certainly accurate to state that not all HLHS patients become opiate dependent or suffer from opiate withdrawal following open heart surgery. As stated, each child's care and needs vary.
Recently, with growing concern and questions surrounding opiate dependency from our families, we reached out to Dr. Moffett, Pharm.D. at Texas Children's Hospital, to lend us insights regarding opiate withdrawal and methadone use in the congenital heart patient.
Methadone Use for Opiate Withdrawal
The most frequently asked questions I have received from parents are regarding ‘withdrawal’ and methadone therapy. There can be a big stigma surrounding the drug methadone, even though it can be very beneficial for children with congenital heart disease who have been in the intensive care unit for long periods of time.
Below, I’ve summarized some of the most common questions I’ve received from parents regarding opiate withdrawal, methadone use, and their child. As always, every child is unique, and the answers to the questions below provide general information. Contact your child’s physician or the clinical pharmacist if you have any questions regarding their medications.
What is opiate withdrawal?
Children who experience opiate withdrawal have often received medications in the intensive care unit, such as morphine or fentanyl, to manage their pain. These medications are in a class of drugs known as opiates. When patients receive these medications in high doses or for long periods of time, they can become ‘tolerant’ to these medications.
If a child has become tolerant to opiate medications, and they are suddenly stopped, a child can experience ‘withdrawal’ from these medications.
What are the signs and symptoms of opiate withdrawal?
Not every child will experience the same signs and symptoms, but common signs and symptoms include: irritability, diarrhea, stuffy nose, nausea or vomiting, poor eating, high blood pressure, or high heart rate.
How is opiate withdrawal prevented?
Typically, if a child has been receiving high doses of opiate medications for long periods of time, slowly reducing the dose of the medication or reducing the number of times per day that the medication is taken will prevent opiate withdrawal. This may occur over days or weeks, and can be done in the hospital or after discharge from the hospital.
Different medications can be used to prevent opiate withdrawal, and methadone is a very common medication used to prevent opiate withdrawal in children with congenital heart surgery.
Why is methadone used for opiate withdrawal?
Methadone is long acting, similar to morphine or fentanyl, and can be taken orally. Therefore, methadone can be used to prevent withdrawal in patients after they have been discharged from the hospital. Since methadone is long acting, the dose can be slowly reduced and the methadone will be slowly eliminated from the body. This helps to prevent the signs and symptoms of withdrawal.
Is there anything special I need to do to get methadone from my pharmacy?
Your child’s doctor may have to fill out a special prescription for you to take to the pharmacy to get methadone. Additionally, some pharmacies may not carry methadone, so it is a good idea to make arrangements prior to being discharged from the hospital so that your child doesn’t miss any doses.
I’ve heard about people using methadone, and they are usually addicted to drugs. Is my child addicted and that’s why he/she is on methadone?
No, in this situation, children are not ‘addicted’ and they don’t get a ‘high’ from the methadone. The dose of methadone is carefully chosen so that patients don’t experience the signs and symptoms of withdrawal, but also don’t feel any other effects. The methadone is helping the child feel as normal as possible.
What things should I watch for while my child is on methadone?
You should contact your child’s physician if they begin to experience any of the signs and symptoms of withdrawal as mentioned above. Additionally, if the dose of methadone is too high, your child might be drowsy or sleeping, or appear sluggish or tired. As always, if there is a change in your child that you are not comfortable with, or have questions about, call your child’s physician.
In conclusion, these questions represent what I have been most commonly asked by parents regarding opiate withdrawal and methadone use for their child. There are always other questions that can come up in your child’s care, so, do not hesitate to ask if something is unclear.
Brady S Moffett, PharmD, MPH
Pain Management and Withdrawal
By: Brady S Moffett, PharmD, MPH
If you've been indoctrinated into the Congenital Heart Defect community, one important lesson learned is that all CHD babies and children are different. As pediatric cardiac surgeon, Dr. Redmond Burke stated, "The babies' hearts are like snowflakes, they are never the same."
One size definitely does not fit all. A particular surgery may be ideal for one HLHS infant, but not for another. The same can be said about medication administration and pain management.
The vast majority of HLHS infants and children undergoing palliation require opiate pain medications (i.e. Fentanyl, Morphine, etc.) following the immediate post-operative period. For various reasons, pain medications may be prolonged causing an infant to become opiate dependent or "hooked."
It is certainly accurate to state that not all HLHS patients become opiate dependent or suffer from opiate withdrawal following open heart surgery. As stated, each child's care and needs vary.
Recently, with growing concern and questions surrounding opiate dependency from our families, we reached out to Dr. Moffett, Pharm.D. at Texas Children's Hospital, to lend us insights regarding opiate withdrawal and methadone use in the congenital heart patient.
Methadone Use for Opiate Withdrawal
by Brady Moffett, PharmD/MPH
The most frequently asked questions I have received from parents are regarding ‘withdrawal’ and methadone therapy. There can be a big stigma surrounding the drug methadone, even though it can be very beneficial for children with congenital heart disease who have been in the intensive care unit for long periods of time.
Below, I’ve summarized some of the most common questions I’ve received from parents regarding opiate withdrawal, methadone use, and their child. As always, every child is unique, and the answers to the questions below provide general information. Contact your child’s physician or the clinical pharmacist if you have any questions regarding their medications.
What is opiate withdrawal?
Children who experience opiate withdrawal have often received medications in the intensive care unit, such as morphine or fentanyl, to manage their pain. These medications are in a class of drugs known as opiates. When patients receive these medications in high doses or for long periods of time, they can become ‘tolerant’ to these medications.
If a child has become tolerant to opiate medications, and they are suddenly stopped, a child can experience ‘withdrawal’ from these medications.
What are the signs and symptoms of opiate withdrawal?
Not every child will experience the same signs and symptoms, but common signs and symptoms include: irritability, diarrhea, stuffy nose, nausea or vomiting, poor eating, high blood pressure, or high heart rate.
How is opiate withdrawal prevented?
Typically, if a child has been receiving high doses of opiate medications for long periods of time, slowly reducing the dose of the medication or reducing the number of times per day that the medication is taken will prevent opiate withdrawal. This may occur over days or weeks, and can be done in the hospital or after discharge from the hospital.
Different medications can be used to prevent opiate withdrawal, and methadone is a very common medication used to prevent opiate withdrawal in children with congenital heart surgery.
Why is methadone used for opiate withdrawal?
Methadone is long acting, similar to morphine or fentanyl, and can be taken orally. Therefore, methadone can be used to prevent withdrawal in patients after they have been discharged from the hospital. Since methadone is long acting, the dose can be slowly reduced and the methadone will be slowly eliminated from the body. This helps to prevent the signs and symptoms of withdrawal.
Is there anything special I need to do to get methadone from my pharmacy?
Your child’s doctor may have to fill out a special prescription for you to take to the pharmacy to get methadone. Additionally, some pharmacies may not carry methadone, so it is a good idea to make arrangements prior to being discharged from the hospital so that your child doesn’t miss any doses.
I’ve heard about people using methadone, and they are usually addicted to drugs. Is my child addicted and that’s why he/she is on methadone?
No, in this situation, children are not ‘addicted’ and they don’t get a ‘high’ from the methadone. The dose of methadone is carefully chosen so that patients don’t experience the signs and symptoms of withdrawal, but also don’t feel any other effects. The methadone is helping the child feel as normal as possible.
What things should I watch for while my child is on methadone?
You should contact your child’s physician if they begin to experience any of the signs and symptoms of withdrawal as mentioned above. Additionally, if the dose of methadone is too high, your child might be drowsy or sleeping, or appear sluggish or tired. As always, if there is a change in your child that you are not comfortable with, or have questions about, call your child’s physician.
In conclusion, these questions represent what I have been most commonly asked by parents regarding opiate withdrawal and methadone use for their child. There are always other questions that can come up in your child’s care, so, do not hesitate to ask if something is unclear.
Brady S Moffett, PharmD, MPH
Thank you, Dr. Moffett, for lending your time and expertise to our HLHS families.
Busy Kiddos and Busy Families
Nutrition Series
By: Emily LaRose, MS, RD, CNSC, CSP, Dietitian at Children's Hospital of Los Angeles
It’s the final week of our National Nutrition Month series! I have really enjoyed working on these posts as a resource for all of the HLHS families out there. In this last post, I am going to review some of the feeding guidelines used after the Fontan operation, and I am going to cover some nutrition tips for older kiddos. As promised, I’m also including a couple of recipes for the whole family to enjoy! The postings I make on this site are my own personal opinions and do not reflect the opinions or views of Children’s Hospital Los Angeles.
Busy Kiddos and Busy Families
Before I get into talking about family nutrition, I wanted to comment on another topic that is specific to our HLHS kiddos: nutrition after the Fontan. I’ve shared some of what we expect and how we provide nutrition for neonates, infants, and toddlers including some centers’ goal weight for the Fontan. After the Fontan, however, some centers have different ways that they may modify a kiddo’s nutritional plan.
Immediately following this third surgical palliation, some hospitals restrict sodium, others restrict fat, most restrict fluids, and some centers do a combination of all of these to prevent some of the post-op complications (including chylothorax) and to facilitate recovery. These restrictions are often temporary, but they can be very important.
At CHLA, we restrict fluids while kiddos are in the hospital after the Fontan. We also put all of our kiddos on a low fat diet for the first six weeks (or so) after their operation. The thought is that by restricting fat, we’re trying to minimize the likelihood of a kiddo developing a chylous effusion (where fat leaks into the space around the lungs) that can sometimes happen because of surgery and pressure changes in the chest.
With the low fat diet, we usually have to acknowledge that kiddos may lose a little bit of weight but, because it’s such a short amount of time, weight loss shouldn’t be too significant. We spend time with families helping to problem solve meals so they have the confidence they need to make low fat foods at home. Again, this modification is usually temporary so once the cardiologist gives a family a thumbs up to resume a normal diet, there aren’t usually any lasting restrictions.
For kiddos on tube feedings, different formulas may be used after the Fontan as well. Tube feeding changes are very individual and can be addressed by your child’s dietitian or medical team.
Once a kiddo is back on his regular diet, we encourage a variety of foods including fruits and veggies, healthy fats, and lean proteins. Some kids do have higher than average nutrition needs so strategies for weight gain can be used but, for the most part, kiddos with HLHS post-Fontan should be following the same general nutrition guidelines as the rest of us.
What about a heart healthy diet?
The idea of a heart healthy diet comes up a lot for our kiddos with heart defects. When we think of a traditional ‘heart healthy’ diet, we think of adults with heart disease risk factors, but having a diet focused on whole foods and healthy fats can be healthy for all of us.
In the years following the Fontan, our goal remains to keep kids healthy and growing. When we think about what a heart healthy diet looks like, a few things come to my mind:
After age two or so, kids don’t need the saturated fats from whole milk anymore so at that point many kids can transition to lower fat or fat free milk.
Healthy fats can come from fish, olive oil, nuts, seeds, avocados, and other non-animal sources. It’s a great idea to get some mixed fats into your family’s diet… and, no, fried foods are not a good source of healthy fats even if a vegetable fat is used.
Don’t overdo it on cheeses and animal fats. Sure, cheese, eggs, and meats can be healthy because they provide protein, vitamins, and minerals, but eating too much of these foods is not good for anyone.
Stay away from heavily processed foods. Processed foods often have a lot of sodium, may have trans fats, and usually don’t offer a whole lot of true nutritional benefit even if the label suggests otherwise.
Eat fresh fruits and veggies! It’s not new or surprising, but providing your family (and kiddos) with a colorful variety of fresh fruits and veggies will provide them with more than just vitamin C and fiber. Plants have a variety of antioxidants that we’re still learning about and most research has said that taking a supplement is not as beneficial as eating food.
We’re busy… what can we do to keep the whole family eating well?
Even with the best of intentions, all of our nutrition and diet goals can be quickly derailed in our busy day-to-day lives. Home cooked meals become fast food burgers and frozen lasagnas for a lot of families. Many parents report that they just don’t have time to cook , don’t know how to cook, or feel that cooking at home is too expensive.
Nutritional benefits aside, there have been a number of studies that have proven that home cooking is usually much more affordable than eating fast food or frozen meals. While I’m a believer that almost anything can exist in a well-rounded diet, I also believe that we should make an effort to eat well most of the time. So what can busy parents do to prevent frequent trips through the drive through?
Plan ahead and shop with a list: Planning a weekly menu can help cut back on grocery shopping time, save money, and prevent food waste. While you’re at the store, it’s also helpful to focus most of your shopping on the perimeter of the store where there are fewer processed foods.
Cook ahead: If you have a few hours once a week to devote to cooking ahead, your food plan can be made much easier. In our house, we spend Sunday afternoons making pasta sauce, roasting veggies, and making meals like beans, lasagna, or enchiladas that can be frozen or refrigerated and reheated for another night during the week when there’s less time to cook.
Get kids involved in cooking: Even young kids can help knead dough, add ingredients to a bowl, or sprinkle salt on a dish. Kitchen tasks can change as kiddos get older and can handle more responsibility. Including kids in cooking makes often them more open to trying new foods that they helped prepare!
Let kids pick out a fruit or veggie at the store: For some parents, bringing kiddos to the grocery store or farmers market and allowing them to pick a new fruit or veggie is a good way for the whole family to try something different. Again, encouraging (and allowing) kids to get involved can be a great way to get them excited about food, eating, and cooking.
What about recipes?
Historically, recipes have come from cookbooks, magazines, friends, and family members, but in the age of the internet, there are even more resources available. The key is finding a few that provide recipes that match your cooking skill level and that you can trust for reliability.
Cookbooks: The Essential Vegetarian by Diana Shaw (now out of print) and How to Cook Everything (by Mark Bittman) are a couple of my favorites. I always figure that it’s easy to make a vegetarian meal non-vegetarian… and Mr. Bittman’s book really does include almost everything.
Websites: I find it helpful to use magazine sites like Bon Appetit, Cooking Light, and Saveur all of whom have kitchens where recipes are well tested prior to publication. I also like the ‘Photograzing’ section of the Serious Eats website (www.seriouseats.com) for finding inspiration. While the pictures provide links to other websites and blogs that may or may not contain recipes, I find it to be like window shopping- I may not buy what’s in the window, but it may inspire me in some other way.
I grew up cooking Southern food alongside my parents, grandparents, aunts, and uncles so, like many others, I have a collection of family recipes that I like to refer to. I also went to culinary school (and have my B.S. in Culinary Arts Nutrition). Because of my cooking family and education background, I cook by inspiration and by feel more than by recipe (but that’s not how I started!).
When I bake I rely on recipes, and I try to keep note what works and what doesn’t. The Joy of Baking website (www.joyofbaking.com by Stephanie Jaworski) is a great go-to site for me. I especially love that all of the recipes have weight measures since when I bake cakes and things, I use a scale.
As promised, I wanted to include a couple of recipes for the whole family so here goes. To give a little bit of background, I have been making various kinds of ‘pockets’ for a few years. I really like that they can be frozen for a quick lunch or dinner on the go. It’s also really easy to make different sizes for your young kiddos (just like an empanada, calzone, or other savory stuffed pastry). I usually fill them with veggies, but you could add meat, chicken, or just about anything else.
Sweet Potato Pockets - With an Indian Flare
For those with kiddos on a low fat diet, I would suggest this first recipe since it can be made with fat free yogurt and fat free milk. Because this is an essentially fat-free dough, it can be a little chewy, but I like it. You can substitute some of the flour for whole wheat if you’d like and, of course, the fillings can be changed to whatever you like. Kids can help mash, mix, and fill these little pastry pockets… though you may end up with a mess. Have fun and feel free to get really creative!
Makes ~10 pockets
Ingredients:
For the pastry dough:
2 ½ cups flour (plus more for rolling out the dough)
½ cup non-fat plain yogurt
½ cup non-fat milk
½ teaspoon salt
For the filling:
1 pound of sweet potatoes, peeled and steamed/roasted
½ cup wilted spinach, cooked or frozen and drained
½ cup peas, cooked or frozen
½ teaspoon salt
Pepper to taste
¼ cup fresh cilantro, chopped (optional)
½ teaspoon of mild curry powder (optional)
2 tablespoons of pepper jelly (optional)
Preparation:
Preheat the oven to 400 degrees.Line a baking tray with parchment paper or a silpat baking sheet.
To prepare the dough, combine flour, yogurt, milk, and salt in a mixing bowl. Gently mix with a fork until it comes together to make a ball of dough. Cover with plastic wrap and allow the dough to rest in the refrigerator.
Prepare the filling by mashing the sweet potatoes with the back of a fork then folding in spinach, peas, salt, and cilantro. You can add black pepper, curry powder, and pepper jelly if you’d like. Taste the filling and adjust the seasoning as desired.
Remove the dough from the refrigerator and divide into about 10 pieces (or more if you’re making smaller pockets). Press or roll each piece of dough into a six inch circle. Add about ¼ cup of filling to each round of dough. Fold the dough in half (into a half moon shape) and fold the edges in or press the edges with a fork to seal them.
Bake the pockets for 20 to 25 minutes or until lightly browned.
A few notes: You could swap out the sweet potatoes for butternut squash or even roasted cauliflower. I do usually add all cooked items to the pockets so that the filling is soft and so that they don’t leak a lot of liquid while they cook. One of our favorites is to make this dough and fill it with wilted spinach, feta cheese, onions, and dill for a little Greek influence. If you’re not following a low fat diet, you can brush the outside with a little olive oil to help the pockets brown in the oven.
Chicken and Black Bean Pockets - Tex-Mex Style
For those who aren’t on a low fat diet, I love the following dough recipe for savory pastries. It does have butter in it so there is some saturated fat but when you break it down into servings, the amount of butter per person actually isn’t too much. I also love the flavor of the olive oil in the crust (and it’s even better with some pepper added to it if your family likes). These are fun to make with kids since there is plenty they can do to help out. And you really can fill these with anything!
Makes ~10 pockets
Ingredients:
For the pastry dough:
1 cup flour (plus more for rolling out the dough)
1 cup cornmeal
5 tablespoons of butter, very cold
¼ cup olive oil plus extra for brushing
1 teaspoon salt
Cold water
For the filling:
1 cup cooked chicken (ground, shredded, or diced chicken is fine)
½ cup black beans, cooked or canned
½ cup corn, frozen or roasted
½ cup salsa
¼ cup fresh cilantro, chopped
Chopped onions (optional)
Shredded cheese (optional)
Preparation:
Preheat the oven to 400 degrees. Line a baking tray with parchment paper or a silpat baking sheet.
To prepare the dough, combine the flour, cornmeal, and salt in a mixing bowl. Cut the butter into small pieces and blend into the flour mixture until it looks like a coarse meal. Gently stir in olive oil. Gradually add cold water until the dough comes together enough to make a ball. Cover the dough and allow it to rest in the refrigerator for at least 30 minutes.
Prepare the filling by mixing all of the ingredients together in a mixing bowl. Taste the filling and adjust the seasoning as desired.
Remove the dough from the refrigerator and divide into about 10 pieces (or more if you’re making smaller pockets). Press or roll each piece into a six inch circle.
Add about ¼ cup of filling to each round of dough. Top the filling with cheese if you’d like. Fold the dough in half (into a half moon shape) and press the edges with a fork to seal them.
Brush the tops of the pockets with a little olive oil. Bake for 20 to 25 minutes or until lightly browned.
A few notes: These are easy to make vegetarian with added veggies or more beans (and without chicken). You could also swap out the chicken for another kind of meat if you’d prefer. This is also a great way to use leftover chicken if you have some in the fridge! I’ve also been known to use this dough to make a larger vegetable pie rolling it out to fit a 9” spring form pan and filling it with all sorts of things.
I have really enjoyed writing these posts for Sisters by Heart; I am honored to have been included in your National Nutrition Month blog series. I hope that the information I have provided has clarified how we think about nutrition for kiddos with HLHS as they grow. All kiddos are different so, as I’ve mentioned, if you have questions or need help with your little one’s nutrition, let your medical team know. I wish you all the best, and Happy Cooking!
Thank you so much, Emily, for all of your fantastic nutritional advice! All of us here at SBH, and the families we serve, have so appreciated your insights!