The Growing (and Sometimes Picky) Toddler
Nutrition Series
By: Emily LaRose, MS, RD, CNSC, CSP, Dietitian at Children's Hospital of Los Angeles
It’s week four of the National Nutrition Month series! Emily LaRose, nutritionist at Children's Hospital Los Angeles, is back again, providing valuable insights into how to navigate the nutritional needs of your cardiac toddler. Thank you, Emily for partnering with Sisters by Heart to share your knowledge and advice with our families!
In this post, I am going to provide some resources and tips to address some of the challenges we face in trying to feed toddlers. We all know that feeding a toddler can be tough! The postings I make on this site are my own personal opinions and do not reflect the opinions or views of Children’s Hospital Los Angeles.
Growing (and Sometimes Picky) ToddlersFeeding a toddler can be a challenge. As kids grow, they develop all sorts of preferences that can change without notice. One day broccoli looks like ‘little trees’ that are fun to eat… and the next day there could be meltdowns about the mere presence of broccoli on a plate. So what is a parent to do?
In short, it is best to stay calm. One of the most important things to keep in mind about feeding a toddler is that eating shouldn’t be a battle. Sometimes toddlers exert the little control they have over their ‘world’ at the dinner table. It’s part of learning and development. In theory, eating is the one thing that a toddler can decide not to do… and there’s not much you can do about it (in the very short term).
There are a number of feeding experts around though Ellyn Satter (http://www.ellynsatter.com/) is widely known for her realistic and practical approach to feeding little ones. She has a great website that’s full of tips for parents of young and picky kiddos, and she has a book called Child of Mine that should be required reading for anyone feeding young kids. I love Ms. Satter’s approach to feeding young kiddos, and I find myself referring to her work often.
When I speak with families, I usually focus on the following as a way to get started:
Make family meals a priority. Your kiddo is going to learn what and how to eat by watching you so eating together (without distractions like T.V. or cell phones) is really important. If you want your kiddo to eat her veggies, you need to eat your veggies… that’s how she’ll learn.
If you want your kiddo to grow up eating a variety of foods, you have to feed him a variety of foods. Your child isn’t going to like everything you give him but, by continuing to offer him a variety of foods, he will be more likely to try new things. Putting some of each of the foods offered at a meal on your toddler’s plate, even if he doesn’t eat them all, is a good way to start.
Be very careful about saying that your kiddo likes or dislikes certain foods. If your toddler hears you say that she doesn’t like spinach, she may not even really know what spinach is but it’s very possible that she will grow up thinking she doesn’t like it.
Make a meal and snack schedule. If your little one doesn’t eat much for breakfast, it’s not a great idea to chase him around the house with cereal or other snacks all morning just to get him to eat something. The best thing you can do it wait until the next meal or snack before you try to feed him something else.
Kids’ tastes change really quickly. Just because your little one doesn’t like something today doesn’t mean she won’t like it two days from now. It’s also important to keep in mind that kids may have to see a new food 10+ times before they’re even willing to try it… and, even then, they may still spit it out a few times before they’re willing to swallow it.
What if my kiddo isn’t gaining enough weight?
Weight gain normally slows after a kiddo turns one. Normal weight gain for kids between one and two years of age is only about 8 grams per day (which is about a pound every month and a half!). Between two and six years of age, weight gain slows down a little more to about 6 grams per day (which is about a pound every two and a half months!).
For kids who have grown well, parents usually find there is less and less pressure on how much weight a kiddo is gaining as long as they’re on a good path. Many times, 15 kilograms (about 33 pounds) is used as a goal weight for the Fontan with many kids reaching this goal sometime between the ages of two and five- but there are plenty of exceptions.
Having the pressure of a weight goal can make feeding feel like uphill battle for some families. Poor heart function, oral motor problems, early feelings of fullness, and other medical problems can make weight gain difficult. With lower weight gain norms, we have a great opportunity for catch-up growth in kids who have had a hard time gaining weight.
All kids grow differently so it’s important to know what is and is not normal for your child. I’m a believer that we can get all kids to grow if we get them enough nutrition, but what works for one may not work for another. Some kids need extra fat, others benefit from more protein and/or carbohydrates.
It’s always okay to ask to meet with a dietitian if you have concerns about your kiddo’s growth or intake. Some doctors will provide you with a referral, and some insurance companies may cover visit costs. Dietitians can help you figure out how to get your little one enough of the right foods to get him growing. Sometimes it takes a little bit of trial and error but, with patience, things will get better.
What about supplement drinks?
Doctors may recommend nutritional supplements to help your kiddo gain weight better. There are plenty to choose from- some with different forms of proteins, carbohydrates, and fats.
The most common supplements for kids who don’t have digestive problems are Pediasure (Abbott) and Boost Kid Essentials (Nestle) but there are a lot of others. Many are milk based so they may not work for kids with allergies; most are lactose-free and should be okay for kids with lactose intolerance. These products have more calories that ‘regular’ cows’ milk because of added sugars and fats, but they have added vitamins and minerals, too.
If you’d prefer, you could try making your own supplement drinks since there isn’t anything truly magical about many of the commercial products. Of course, it’s a good idea to check with your kiddo’s pediatrician (or dietitian) first just to get an okay.
I’ve included a couple of sample recipes, but I wouldn’t use either as a kiddo’s only source of nutrition. Either one could be added to his or her diet as a ‘boost.’ There are a lot of resources out there with recipes, but these are a couple that I have had success with.
If you were to blend the following foods you would have a drink with a few more calories and about the same amount of protein as a bottle of Pediasure (248 calories vs. 240 calories both with ~7g protein).
6 ounces of whole milk
½ of a ripe banana
2 teaspoons of honey
1 teaspoon of flaxseed oil
For another example, you could blend the following items for a drink with a few more calories and about the same amount of protein as a bottle of Boost Kid Essentials 1.5 (366 calories vs. 360 calories both with ~10g protein).
6 ounces of whole milk
¼ cup of cooked/mashed sweet potatoes
1 tablespoon of honey
1 tablespoon of almond butter
1 teaspoon of flaxseed oil
Since these recipes are small, you may need to make larger batches to accommodate your blender or food processor; you can always refrigerate any extra for later. As another option, you could use baby foods that mix into milk really easily. The options are endless so feel free to get creative; adding cinnamon, nut butters, chocolate powder, and berries are all good options- but don’t stop there!
If you were going to use almond milk, rice milk, or another type of dairy milk substitute, the recipe would not provide as many calories or as much protein as the ones I’ve included here. Using nut butters, cooked eggs, tofu, avocado, and other additives can help to fill in the gaps- your dietitian can help you figure out your best options.
*** If your kiddo is on tube feedings, always discuss any proposed changes with your child’s doctor or dietitian before you make any changes. The recipes I’ve included are not intended as tube feeding formula replacements.
What if my kid is on tube feedings?
For kiddos who are on tube feedings, we make adjustments for growth a little bit differently. Sometimes we will try new formulas to see if we can get a kiddo growing with a different mixture of fats or by giving different proteins. Sometimes we’ll change the timing of feedings or give some feedings overnight while the kiddo is sleeping. Sometimes we can add foods to tube feedings to help with weight gain, too.
Does my child need to take a multivitamin?
With a normal and varied diet, most kids probably don’t need to be on a special multivitamin, but it’s always a good idea to ask your child’s pediatrician about what may be best for your kiddo. If needed, most physicians will suggest a once-a-day chewable vitamin or something similar.
I’m partial to vitamin products without a lot of sugar or extra filler ingredients. I don’t usually recommend gummy vitamins for a few reasons (though we get asked often).
Gummy vitamins can be a choking hazard because young children tend not to chew them very well.
They tend to stick in kiddos’ teeth and can cause dental problems. Since we worry a lot about the mouth being a possible place where infections can start (especially for cardiac kiddos), we try not to encourage anything that can cause decay and other problems.
Dosage recommendations for gummy vitamins are usually between two and six per day (depending upon the brand) and, truly, no one needs to eat candy as a daily supplement.
They usually are not complete sources of vitamins and minerals. Many of the powdered or chewable vitamins have better amounts of all of the micronutrients we’re looking for.
As the package says, always keep vitamins out of reach of small children; overdoses can be fatal.
The Cardiac Infant
Nutrition Series
By: Emily LaRose, MS, RD, CNSC, CSP, Dietitian at Children's Hospital of Los Angeles
We're continuing on with our Nutrition Series this week, with the help of resident expert Emily LaRose, dietitian at Children's Hospital Los Angeles. Today, Emily discusses the nutritional concerns of the cardiac infant into early toddlerhood. Thank you, Emily for continuing to share your knowledge and advice with our families!
I’m back for week two of the National Nutrition Month series! In this post, I’m very excited to write about what happens for baby’s nutrition once he is discharged home from the hospital the first time. This post will take us through starting solids and transitioning to cow’s milk. The postings I make on this site are my own personal opinions and do not reflect the opinions or views of Children’s Hospital Los Angeles.
As I’d mentioned in my last post, nutrition and growth are both big parts of the interstage period. While we can establish a nutrition plan in the hospital, our plans may change once a baby has had some time at home so we’re always ready to make adjustments. Once babies are home, we rely on parents to tell us what is and isn’t working.
We focus a lot on growth and weight gain in the interstage period because babies who grow well tend to stay healthier, do better with their future surgeries, and have better overall development than those who haven’t grown as well. A good nutritional foundation helps with the body’s response to surgery and with healing afterward. Good nutrition also helps with immune function and brain development.
After the Glenn, weight gain and growth are generally less of a concern for a few reasons:
• Babies tend to gain weight a little more easily after then Glenn than in the interstage period.
• The blood flow to the baby’s belly is usually more stable so digestive problems are usually less of an issue.
• There isn’t as much focus on rapid growth because there usually isn’t another surgery planned for the near future (since the Fontan is usually many months away).
After the Glenn, we are still trying to get babies to grow (so we do usually continue with high calorie breastmilk or formula) but, in a lot of ways, post-Glenn nutrition becomes more like ‘typical’ baby nutrition. Babies progress toward taking solid foods, develop regular eating schedules, and eventually start taking cow’s milk just like other babies.
So going forward how much weight gain should we expect?
As I’d mentioned before, usually we say that weight gain of 20 to 30 grams per day (five to seven ounces per week) is normal for babies for the first three months or so. But, after the first few months, growth goals for the remainder of the first year are very individual for kiddos with HLHS.
There are standard growth goals, but if a baby gets a slower start, he may go through periods of faster growth (which we call ‘catch-up growth’). If a baby gets sick or spends some extra time in the hospital, she may grow a little more slowly for awhile before her weight gain picks up. Again, there is no set way that all kiddos grow, but sometimes averages can help us figure out how things are going.
For growth goals, the following will give you an idea of what would be average, but keep in mind that your kiddo may be growing on his or her own curve.
• 3 to 6 months: average weight gain may slow down a little to an average of about 18 grams per day (about four to six ounces per week). Length gains should be about 0.5 centimeters per week (or about an inch every five weeks).
• 6 to 12 months: weight gain slows down a little more to an average of about 12 grams per day (about three ounces per week). Length gains also slow down a little more to about 0.3 centimeters per week (or about an inch every seven or eight weeks).
Another good rule of thumb for weight gain is that a baby should double her birth weight by six months and triple it by one year. So if your little one was born at seven pounds, she should be about 14 pounds at six months, and about 21 pounds at her first birthday- if everything goes exactly according to plan.
When can I start giving my baby solids?
People ask about when to start babies on solids all the time… and, unfortunately, there are a lot of different answers. The American Academy of Pediatrics recommends solely breastfeeding for the first six months of age though multiple other sources suggest that between four and six months is a good age to start solid foods. Giving solid foods is not recommended for infants less than four months of age.
For an HLHS kiddo, cardiologists will often suggest that families wait to start a baby on solids after her Glenn but that isn’t always the rule. If you’re thinking that your little one may be ready to try some solid foods, talking to your baby’s cardiologist and pediatrician is a good idea.
The way the solids are introduced to an HLHS infant is just like a non-cardiac baby. Basically, we rely on the baby to tell us when he’s ready and we go from there. For more information, this website (http://www.healthychildren.org/English/ages-stages/baby/feeding-nutrition/Pages/default.aspx) was created by the American Academy of Pediatrics and is a great resource. They have covered everything from how to know if your baby is ready for solids, what kinds of foods are good to start with, how much to give, and much more. They have even included a sample menu that could be helpful for older babies.
A few things to remember:
• If your baby turns her head away and refuses to eat, don’t force her. It’s okay to wait to try solid foods another day.
• Your baby will learn to eat by watching other people eat. Include your baby in family meals and feed him when other people are eating.
• Babies are messy eaters, but that’s how they learn to eat. It is normal for meals to end up on the baby’s clothes, bib, and face.
• Your baby isn’t going to like all of the foods that you offer her but tastes change quickly so it’s okay to repeat a food a few days later. You may be surprised with what happens!
• We always want to make sure our cardiac babies are safe so if you notice that your baby is coughing, gagging, or choking with his feedings, check in with his medical team to make sure that you are okay to continue.
• If your baby has a feeding tube, he may be able to have some solids added to his feeding plan as well. Once he is at the right age and developmental level for solids, ask your dietitian, cardiologist, and/or pediatrician if this may be an option for your kiddo.
What about food allergies?
Allergies are an important subject since food allergies have become more common in recent years. No one knows what is leading to so many more cases of food allergy, but everything from household cleaners and antibiotics to environmental changes and genetically modified foods has been blamed. At this point, we just don’t know (and, in my opinion, there are probably many factors at play).
While the current American Academy of Pediatrics feeding guidelines don’t specifically address when to introduce allergenic foods to babies, some of the most current academic papers (including one published earlier this year in the Journal of Allergy & Clinical Immunology: In Practice) on prevention of food allergies suggest starting highly allergenic foods like soy, wheat, shellfish, and even tree nuts early on.
Recommendations are always changing so, again, this is something you will want to talk to your kiddo’s pediatrician about.
How do I transition my baby from a bottle-feeding schedule to a meal schedule?
As your baby grows, solid foods will play a larger and larger role in his nutrition plan; the goal remains to get the baby to grow as normally as possible. It’s important to remember that all babies and kiddos are different so allowing them to develop at their own pace is important.
Some babies wean themselves off of the bottle and transition to meals all by themselves. They can be so excited about meals that the bottles fall away and sippy cups of milk fill in where some of the bottles once were. Other kiddos demand a more gradual transition.
If you’re having trouble, I often suggest that parents write out the baby’s schedule (of meals and bottles). At around one year, she will probably need four or five meals per day (of solids) to keep her energy levels up and to keep her growing normally. If she is taking four or five bottles per day, but only taking solids two times per day, replacing once bottle at a time with a meal or snack is a good place to start if your medical team is okay with it.
A few other things that may help include the following:
• When you can, eat with her so that she knows that it is mealtime.
• It can help to offer solids first and then formula or milk so that she’s not too full for her ‘big girl’ meals.
• You can make a schedule change every few days (give or take) to get her onto her grown up schedule.
• We try to wean babies off of the bottle between 12 to 14 months so encouraging them to use a cup earlier on really helps (if they’re ready).
We see many picky eaters in the next stage of development. When kiddos aren’t growing well or when parents worry about whether or not kids are getting enough nutrition in, the question of supplmental drinks often arises. Stay tuned for my next post which focuses on feeding our picky cardiac toddlers.
The Cardiac Newborn
Nutrition Series
By: Emily LaRose, MS, RD, CNSC, CSP, Dietitian at Children's Hospital of Los Angeles
Nutrition and related weight gain are major issues for most of our HLHSers, and for cardiac babies in general. In recognition of Nutrition Month, we have an incredible nutrition series brought to you by Emily LaRose - dietitian at Children's Hospital Los Angeles. Emily's opening post provides a comprehensive look at several nutritional concerns and covers cardiac nutrition from birth to surgery and beyond. Thank you so much Emily for taking the time to provide our families such excellent analysis!
Emily is the dietitian in the Cardiothoracic Intensive Care Unit at Children’s Hospital Los Angeles where she works with the medical team and families to provide nutrition for kiddos before and after cardiac surgery.
Over my nearly 10 years as a registered dietitian, I have worked with children and adults of all ages. After completing the Neonatal Nutrition Fellowship at Texas Children’s Hospital in 2006, I knew that I was destined to focus on working with infants and young kiddos. I began in my current role in 2009 and, while I’ve seen a lot, I continue to learn from patients and families all the time. I am part of a great medical team, and I am in regular contact with colleagues from different hospitals across the country. Together, we can all work to understand how to help cardiac kiddos grow and thrive.
I have met so many wonderful families that serve as ongoing inspiration for the work our team does everyday. I am honored to share some of my professional experience with the Sisters by Heart community; I hope you find it helpful. The postings I make on this site are my own personal opinions and do not reflect the opinions or views of Children’s Hospital Los Angeles.
Since I will be covering a variety of HLHS nutrition topics over the next couple of weeks, I thought that it would make sense to divide the postings by age: the cardiac newborn, infancy into toddler-hood, growing (and sometimes picky) toddlers, and busy school age kiddos. Happy National Nutrition Month!
The Cardiac Newborn
Usually when babies are admitted to our cardiac intensive care unit, I try to meet with parents to review how we give nutrition to these little ones before and after surgery. With moms who may still be in the birth hospital and dads who may be shuttling back and forth between hospitals and home, it can sometimes take a little while before we’re able to speak but, all the while, we’re getting nutrition into these little ones as best as we can.
In our first visit, I review how we give nutrition to cardiac babies, and I try to make sure that moms have the support they need to get pumping if they’re planning to feed the baby breastmilk when the time comes. Often we talk about the progression of nutrition from IV nutrition to oral feedings and everything that comes in between. I also talk a little about my role as the dietitian on our ICU team since a lot of people aren’t familiar with what a dietitian may do when kiddos aren’t eating.
I thought for this first post I would review some of the nutrition highlights for the cardiac newborn during his or her first hospitalization. A lot of this information comes directly from what I talk to new parents about so that they know what the nutrition plan is… and so that in the midst of everything going on with the baby, they know that we’re doing what we can to help the baby heal and grow.
The Nutrition Plan
Because blood flow to an HLHS baby’s intestines may not be stable or adequate, intravenous (IV) nutrition is often the first, and possibly only, source of nutrition for these little ones before surgery. You may hear this called parenteral nutrition (PN) or total parenteral nutrition (TPN); you may hear the word Intralipid as well. All of these descriptions are talking about the dextrose (sugar/carbohydrate), amino acids (protein), and fat (Intralipid) as well as vitamins, minerals, electrolytes, and other additives that can be given through a vein when feeding into a baby’s tummy isn’t possible.
We can actually get all of the nutrition that a baby needs into a tiny yellow bag and a little white syringe. It’s not a perfect system (we’d rather feed into baby’s tummy when we can), but it’s a lifesaver- literally.
Once deemed safe, many hospitals have feeding protocols that dictate how and when to start feeding into the baby’s tummy (while the IV nutrition continues). Most of the time, feedings are started through a small tube that is placed in the baby’s nose or mouth with a tip that sits either in the stomach or in the small intestine.
With the feeding tube in the stomach, feedings may be started continuously (given 24 hours per day) or as small volume bolus feedings every three hours or so- there is no real consensus on which way is better. With a feeding tube in baby’s intestine, feeds are given continuously. Eventually, these tube feedings are gradually increased (and the IV nutrition decreased) to meet the baby’s energy and protein needs.
Feeding progress is usually very slow because tummy problems can be common with HLHS. Babies may have slowed digestion after surgery or abnormal blood flow to their intestines. They may spit up, have bloody stools, or may be excessively fussy. While some of these problems may be unavoidable, studies have told us that if we have a gradual feeding plan that we stick with, we can avoid some of these symptoms and make faster progress in the long run. If we rush a baby to get more nutrition than he or she is ready for, sometimes we end up taking one step forward followed by many steps back.
So when we start feedings, what will we use?
Amy, Michelle, and Karen gave excellent perspectives on breastmilk and breastfeeding earlier this month. Breastmilk is so amazing and provides so many immune factors, micronutrients, special fats, healthy bacteria, and other benefits to these little ones. It is super easy to digest, and there are a number of studies out there that talk about how breastmilk can help to prevent some of the digestive problems that preemies and HLHS babies are known for. It’s truly customized nutrition that formula will never match!
For some moms, however, providing breastmilk may not be an option. Breast surgery, postnatal complications, certain medical conditions, some medications, and a variety of other factors may make breastfeeding difficult or impossible. Some moms choose not to breastfeed and that is okay, too.
Using donor breastmilk (from one of the nationally recognized milk banks) can be a good option for especially sensitive infants though it is rarely used long term. When breastmilk isn’t an option, there are plenty of formulas available for feeding infants with HLHS or for adding calories and protein to breastmilk (fortifying) when needed.
Some hospitals recommend standard formulas (like Enfamil Premium or Similac Advance) while others use semi-elemental or partially hydrolyzed formulas (like Pregestimil, Nutramigen, or Alimentum) in their feeding protocols. In some cases, even more broken down (elemental) formulas like Elecare or Neocate are needed. When we’re deciding which formula to use, blood flow to the baby’s belly, prematurity (and birth weight), GI problems or surgeries, and other medical conditions are all things we think about.
Are there cases where breastmilk or one of these formulas can’t be used?
As Michelle and Karen mentioned, chylothorax (or chylous effusion) can add an extra challenge when we’re talking about feeding babies with HLHS. Chylothorax can actually happen as a result of any surgery around the heart, and treatment almost always includes diet modification. The primary challenge is to find a way to get the long chain fat out of the baby’s diet while still getting him enough calories to grow. Unfortunately, long chain fat is the primary fat in breastmilk and infant formula.
IV nutrition is an option and may be used in some cases though, as I’ve mentioned, we try to feed into a baby’s tummy when we can. Skimmed breastmilk may be an option if enough fat can be removed; other formulas and special types of fat can then be added to the milk so that the infant has what she needs to grow.
If skimmed breastmilk isn’t an option, special formulas (like Enfaport, Monogen, and many others) can be used for oral or tube feedings until the drainage stops. Treatment usually continues for another two to 10 weeks until the cardiologist is confident that the area where the leak occurred is fully healed.
When can babies start to take feedings by mouth?
As babies recover, their tube feedings will increase and the breathing tube will come out. Once a baby is fully awake and his or her breathing is stable, we will start to think about letting the baby try some feedings by mouth- usually from a bottle.
Occupational therapists and speech language pathologists may evaluate if the baby is ready, able, and willing to take some nutrition by mouth. They will come up with treatment plans to help the baby progress to oral feeding as long as the baby is safe to do so. They observe babies as they eat and work with families to figure out how a baby is responding to feedings- is he sweating a lot, is her breathing rate increasing, is he working too hard, is she able to suck-swallow-breathe safely?
If a baby has a weak cry or is coughing or gagging with his feedings, swallow studies may be ordered to make sure that the breastmilk or formula isn’t going down the airway (aspiration). In some cases, positional feeding techniques are used to prevent aspiration. Sometimes feedings may be thickened (using baby cereal or other thickeners) if the baby is aspirating with thin liquids. For some infants, aspiration makes feeding by mouth unsafe and long-term tube feedings are needed.
With practice, the hope is that the baby will begin to take more and more nutrition by mouth relying less on the feeding tube. For some babies, eating causes a lot of stress so they may be limited to oral feeding a couple of times per day or for a small amount of time per feeding until they get stronger.
Once the team is confident that the baby is able to eat enough to stay hydrated, we will start talking about taking the feeding tube out. Some babies learn to take all of their feedings by mouth within a couple of weeks and others take much longer. Unfortunately, we don’t have great ways to predict who will eat well and who will not. When a baby can’t eat enough by mouth, but is otherwise ready for discharge, the team may recommend that he go home with full or partial tube feedings.
So how much nutrition do cardiac babies really need?
We have all sorts of ways that we can estimate how much nutrition someone may need- from babies and toddlers to older kids and adults. There are standard calorie levels for term babies without medical conditions as well as standards for premature babies. All babies are different and what works for one may not work for another. Ultimately, for HLHS babies, we rely on four things to give us hints about what a baby’s nutrition needs may be: research, previous experience, healing, and growth.
Research tells us that right after cardiac surgery babies have reduced calorie needs. The physical stress that their little bodies go through causes their metabolism to hibernate (sort of) for a week or so. After they recover, their nutrition needs increase, and, if they’ve been on bypass, they increase a lot.
Most research suggests that infants with HLHS often require upwards of 10 to 30% more than other term infants though there are infants who grow well on far less than we’d expect (and some who require even more). Energy needs depend upon how well the baby is able to eat, if he or she is able to absorb the nutrition their being given, how hard he or she is working to breathe, any other medical conditions, and much more.
We think of breastmilk as having about 20 calories per ounce on average though there can be a lot of variability. Standard formula dilution, with a few exceptions, is also 20 calories per ounce. For our HLHS babies, we usually find that breastmilk and formula needs to be mixed to at least 24 calories per ounce for babies to grow- but not always. Sometimes we will increase calories even further to 27 or even 30 calories per ounce to get babies to grow.
In addition to some of the formulas I’d mentioned, hind milk feedings, skimmed fat (from mom’s breastmilk), other protein, fat, and carbohydrate additives may be used to change the nutrition profile or increase the calories in breastmilk or formula.
Ultimately, the baby will tell us how much nutrition he or she needs to grow and thrive. All babies are a little different and, like medicine, nutrition isn’t an exact science.
What is normal growth for an HLHS baby?
Weight loss just after birth is normal for all babies. Usually, up to about 10% is expected with the goal of baby regaining his or her birth weight by two weeks of age. But what is normal for a baby who has had surgery or who has relied on nutrition support? It’s tough to say and can vary greatly.
Often, when we’re talking about weight gain for a newborn baby, we’re looking for about 20 to 30 grams per day (or about five to seven ounces per week) after the first two weeks of life. We’re also expecting newborns to grow in length by 1.5 to 2.5 centimeters (1/2 to 1 inch) per month. Again, these are general goals for all newborn babies; more weight growth may be normal for some babies, less may be normal for others, it depends.
Another consideration is to look at how proportionate a baby is using weight-for-length growth standards (charts). If a baby is gaining weight well but is not growing longer, he may appear chubbier than other babies his age. If a baby is gaining weight normally but is growing in length faster than most babies, she may appear thin. Despite the average standards we use, gaining 15 grams a day may be normal for some babies while gaining 40 grams a day may be ideal for others.
If an infant is getting enough nutrition, in theory these growth goals should be possible. Unfortunately, that still doesn’t mean that growth is easy or the same for all babies. Getting enough nutrition to show good growth before it’s time for another surgery is vital, and I know that HLHS babies (and parents) work really hard for every ounce.
Things to think about
1. If you want to breastfeed, start pumping early on to establish your milk supply and continue pumping 8-10 times each day. Babies usually eat every 2 to 3 hours so pumping on a similar schedule will remind your body to keep making milk even if you baby isn’t feeding just yet. Breastmilk can be frozen for about 6 months in a regular freezer but make sure to date it so you are sure to use the older milk first.
2. Right after birth through about a week or two after surgery, a cardiac baby’s weights often do crazy things. We see weight loss in the beginning, a lot of weight gain with fluids, weight loss again… it’s a rollercoaster! A couple of weeks after surgery is usually a good time to start looking at what your baby’s weight is doing. He or she may not be gaining weight by leaps and bounds, but the average trend should be positive.
3. Be patient. Even if everything goes perfectly, it takes awhile for an HLHS baby to get to full feedings (by tube or by mouth); if we rush the process, we often have to backtrack. Keep in mind that when babies are born, it takes time for them to learn to eat. HLHS babies have some extra challenges including higher nutrition needs, different breathing requirements, a heart that’s working with fewer parts, digestive problems, recent surgery, etc.
4. A weight gain goal of 20 to 30 grams per day is a guideline but may not be the right amount of weight gain for all babies. Looking at weight for length on growth charts can be a really helpful way to make sure that a baby is gaining weight proportionately over time. Your pediatrician (or dietitian) has these growth charts if you want to see them.
5. All babies are different and it’s always okay to ask questions! If you haven’t met a dietitian and would like to- just ask! If you have questions about your baby’s nutrition or other medical conditions- just ask! We’re all here to help.
Breastfeeding the HLHS Baby - the Practitioner Perspective
Nutrition Series
Michelle Steltzer, CPNP-AC, Cardiovascular Program Nurse Practitioner
On Monday, one our Sisters by Heart moms, Amy, shared the parent perspective on the question of whether it’s possible to breastfeed an HLHS baby. Today, we are fortunate enough to have two seasoned practitioners from Boston Children’s Hospital provide their perspective on breastfeeding an HLHS baby!
Michelle Steltzer, CPNP-AC
Cardiovascular Program Nurse Practitioner
Michelle is currently working on publishing a case study on a breastfeeding HLHSer who transitioned to fully breastfeeding during the interstage period with excellent growth.
It is an honor to share my perspective with Sisters by Heart and I truly appreciate all the work that you do each day to reach out, connect, and support families with HLHS. As mentioned, the congenital heart disease population is near and dear to my heart having worked many years as a bedside nurse in the ICU and in 1999 as a cardiology nurse practitioner in the ICU/ward at Children's Hospital of Wisconsin/Medical College of Wisconsin (1993-2007). I transitioned to a cardiovascular surgery nurse practitioner on the ward at Boston Children’s Hospital 5 years ago. Through the years, I have written a lot about nutrition, spoken at national and local conferences, and gained much experiential practical knowledge at the bedside with amazing insight provided by great patients and families like you folks struggling with feeding, growth, and nutrition. I am happy to share my perspective with you and trust you find it useful.
On a daily basis, I am inspired by the dedication and passion of so many families that ensure the benefits of breast milk are available for their infant via breast feeding, expressed breast milk by bottle, and/ or other tube feedings. As a mother of two children that breastfed both infants until going back to work, it is no simple request for any parent. Breastfeeding is a lot of hard work and requires much dedication and support by the entire family to ensure success. Currently, as Amy mentioned, I am working on writing up a case study that will give a detailed description of one mom’s successful transition to breastfeeding during the interstage period. To give you perspective, I walked to the patient’s bedside following morning rounds report by my NP colleagues after not seeing this particular infant since the initial newborn surgical hospital stay. Upon seeing the infant, I promptly walked out of the room thinking to myself, “This patient cannot possibly be the patient advertised during sign out by my peers that recently had a Glenn surgery. I must be in the wrong patient room.” Needless to say, I was completely wrong in my presumption and will share more details in a journal publication in the future about this practice changing experience.
One key to success, particularly in the CHD population, is reaching out and truly engaging all members involved in your infant’s care team that is rallying for successful growth and nutrition. This includes: first and foremost the family, pediatrician, referring and primary cardiologist, hospital teams (prenatally, postnatally in CICU, floor wards, and follow-up clinic visits), early intervention, speech/feeding therapy, and cardiac developmental centers available at your institution/region. These team players (from nursing, lactation, nutrition, MD, therapists, etc) along with family dedication are essential to ongoing success with breastfeeding for this high risk and fragile population - particularly during the interstage period. This period is often described as a very isolating experience for the family, particularly for a dedicated breastfeeding mother. Thoughtful discussions with mothers and families throughout all care opportunities with health care providers are critical to ensure the best outcome for the infant and family.
As Amy mentioned, breastfeeding and oral feeding in general is a lot of work and a "stress test,” particularly for infants with HLHS. Realizing this at baseline is important because there can be additional complicating morbidity factors that may impact the stress of feeding. Some of these concerns are: poor ventricular function, valve regurgitation, breathing fast due to too much blood flow or other respiratory concerns, vocal cord injury, oral aversion, reflux, other non-cardiac anomalies, and other morbidity factors that may contribute to an infant's failure to thrive and grow. Having said that, these factors should not limit the decision to utilize breast milk and all its beneficial immune properties.
Discussions with health care providers about breastfeeding and utilizing your precious breast milk is essential. It is also important to note, that there are some special cases such as chylous effusion (milky appearing fluid accumulating or draining around the lungs), milk protein allergy, or guiac positive (bloody) stools that may require alternative supports for nutrition. In these instances, a conversation about alternative options and adjustment in the breast milk diet may need to occur in the short term period.
Practical 5 Pearls of Wisdom to Share with Moms Interested in Breastfeeding
1. Discuss prenatally and postnatally your thoughts on breastfeeding. On a daily basis bring up your desire to encourage breastfeeding and connect with all your lactation resources early.
2. Keep your breast milk supply up drinking proper fluids and frequent pumping at least every 3 hours. If concerned, please reach out to your lactation consultant early. This way you will have plenty of that nutrient rich milk with all its beneficial immune properties when your baby is ready. *Please see below our lactation consultant expert from Boston Children’s Hospital, Karen Sussman-Karten’s input for other pearls of wisdom on breast milk supply and “lactoengineering.”
3. Practice patience and persistence. Never miss an opportunity to practice. Try to breastfeed or even just work on non-nutritive suck if your team agrees during the inpatient stay (preoperatively if possible) and outpatient. In some cases, you may need to be persistent in your requests to try breastfeeding, but don't be shy in speaking up for your baby. Once your child is on bolus feedings, there are at least 8 feeds at least in a day and thus 8 times to practice daily with the health care team and ultimately the primary feeders of the infant after discharge.
4. Advocate and utilize the resources available to you in the home surveillance monitoring program (saturations, heart rate, daily weights, and logging the number, volume, and length of feeds-particularly if breastfeeding).
It continues to be an issue among some institutions that insurances will not cover scales. Advocate early with your primary team, ask for scales that weigh to at least 10grams (there are many on the market), and if possible consider scales that weigh to <10 grams.
Communicate honestly with your providers about how the breastfeeding and growth is progressing. It is important to share with your providers if you are noticing fatigue, sweating or diaphoresis during feedings because these may be a sign that your baby is working too hard to feed to adequately grow and thrive.
Avoid feeding (by bottle or breast) longer than 20-30 minutes to minimize losing more calories during the feeding process than actually gaining. There are some weeks where you may need to add more bottle feeds due to your family circumstances or or infant’s illness. Make sure to pay particularly close attention to your baby’s progress with your home scale. These periods may warrant more detailed intake and should not be thought of as a failure to breastfeed successfully.
Remember the nature of shunt dependent blood flow in HLHS heightens your infant’s vulnerability during the interstage period, and this is the primary reason why home surveillance monitoring was introduced over a decade ago. In some cases, your infant may require to be seen by your local providers (cardiology or pediatrician) or visit the emergency room for reassessment of plan of care. Some instances may require readmission for closer monitoring of feeding and cardiovascular status. This is by no means a failure on your part, but the “nature of the disease process of HLHS.”
5. Be practical with your expectations. Don't expect your baby to fully breastfeed by the time of first discharge following stage 1 palliation (whether it is Norwood with BT shunt, Sano with right ventricular to pulmonary artery homograft, or Hybrid). Lastly, please remember that you are not alone, take care of yourself, and never give up!
Karen Sussman-Karten, RN, IBCLC
Karen is a Lactation Consultant in the Lactation Support Program at Boston Children’s Hospital and is currently the Board Chair of the Mother’s Milk Bank of New England.
Amy and Michelle have shared so much valuable wisdom about breastfeeding and providing breastmilk for CHD babies. I have been a lactation consultant at Boston Children’s Hospital since 2006 and I have a few more thoughts for you.
Having adequate milk production is the foundation for success. Without it your options are limited. Since your baby will probably not be able to breastfeed in the first few days, expressing milk is essential to establish milk production. It’s important to start as soon after delivery as possible. Pumping frequently, every 2-4 hours is recommended. You may be able to collect more milk with manual expression in those early days. “Hands on pumping,” massaging and compressing while using a breast pump, can also result in collecting more milk.
Think of your early breastfeeding attempts as practice sessions. Don’t expect your baby to drink large volumes at the breast initially. Try not to get discouraged; practicing will lead to improvement over time and the skin to skin contact can help with milk production and breastfeeding.
Once your baby seems to be drinking at the breast, doing a pre and post feed weight to measure intake can be helpful, particularly in the hospital when you have access to use a very accurate scale for pre and post weights. As mentioned by Amy, our parent expert, most baby scales intended for daily weight checks are not sensitive enough to weigh less than 10 grams. Of course purchasing an accurate scale can be costly. You may want to consider renting one like the Medela baby weigh scale for home based on your infant’s progression with breastfeeding. It’s very important to keep your baby in the same clothing and diaper for the pre and post weight. Changing the diaper or weighing your baby naked will not give accurate results.
“Lactoengineering” refers to ways of altering the breast milk or breastfeeding to meet your CHD baby’s specific needs. Since getting the most calories is a major concern, there are some techniques you can use to increase caloric intake. The caloric content of your breast milk can be tested using a creamatocrit machine or milk analyzer. Some hospitals have this equipment. The assumption is that breast milk has 20 calories per ounce but when tested it is often higher. This becomes important if your infant’s EBM is being fortified above 20 calories per ounce, potentially up to 26 or 28 or more calories per ounce. Some infants do not tolerate the additives for a higher calorie diet so it can be very helpful to know the general caloric density of your breast milk as a baseline. Sometimes the additives can be reduced or eliminated depending on the results. Beware, the fat content of your milk varies throughout the day so testing once is like a snapshot of the calories per ounce.
Another interesting phenomenon is that the fat content of your milk increases toward the end of a nursing or pumping session. If you make more milk than your baby drinks, you can use more of the fat rich “hindmilk” to increase the calories. You can pump for the first 3 minutes and freeze that “foremilk” for later use. Then either nurse your baby or pump the remainder of the “hindmilk” and use only that.
If your baby has a chylous effusion, they cannot tolerate the fat portion (long chain fatty acids) in breast milk. It is possible to separate the fat from your milk and use the “skimmed” breastmilk. This can be done with a centrifuge machine or with other methods of allowing the milk to separate and removing the cream layer. This “skimmed” breast milk will need to have other oils and nutrients added to make up for the calories lost by removing the cream. This allows your baby to continue receiving your milk rather than a special formula while they have a chylous effusion.
Thank you so much, Michelle and Karen for your helpful insights into breastfeeding a child with a complex congenital heart defect like HLHS!
Stay tuned for next week’s post in our nutrition series, “The Cardiac Newborn!”
Breastfeeding the HLHS Baby - the Practitioner Perspective
Nutrition Series
By: Michelle Steltzer, CPNP-AC, Cardiovascular Program Nurse Practitioner
On Monday, one our Sisters by Heart moms, Amy, shared the parent perspective on the question of whether it’s possible to breastfeed an HLHS baby. Today, we are fortunate enough to have two seasoned practitioners from Boston Children’s Hospital provide their perspective on breastfeeding an HLHS baby!
Michelle Steltzer, CPNP-AC
Cardiovascular Program Nurse Practitioner
Michelle is currently working on publishing a case study on a breastfeeding HLHSer who transitioned to fully breastfeeding during the interstage period with excellent growth.
It is an honor to share my perspective with Sisters by Heart and I truly appreciate all the work that you do each day to reach out, connect, and support families with HLHS. As mentioned, the congenital heart disease population is near and dear to my heart having worked many years as a bedside nurse in the ICU and in 1999 as a cardiology nurse practitioner in the ICU/ward at Children's Hospital of Wisconsin/Medical College of Wisconsin (1993-2007). I transitioned to a cardiovascular surgery nurse practitioner on the ward at Boston Children’s Hospital 5 years ago. Through the years, I have written a lot about nutrition, spoken at national and local conferences, and gained much experiential practical knowledge at the bedside with amazing insight provided by great patients and families like you folks struggling with feeding, growth, and nutrition. I am happy to share my perspective with you and trust you find it useful.
On a daily basis, I am inspired by the dedication and passion of so many families that ensure the benefits of breast milk are available for their infant via breast feeding, expressed breast milk by bottle, and/ or other tube feedings. As a mother of two children that breastfed both infants until going back to work, it is no simple request for any parent. Breastfeeding is a lot of hard work and requires much dedication and support by the entire family to ensure success. Currently, as Amy mentioned, I am working on writing up a case study that will give a detailed description of one mom’s successful transition to breastfeeding during the interstage period. To give you perspective, I walked to the patient’s bedside following morning rounds report by my NP colleagues after not seeing this particular infant since the initial newborn surgical hospital stay. Upon seeing the infant, I promptly walked out of the room thinking to myself, “This patient cannot possibly be the patient advertised during sign out by my peers that recently had a Glenn surgery. I must be in the wrong patient room.” Needless to say, I was completely wrong in my presumption and will share more details in a journal publication in the future about this practice changing experience.
One key to success, particularly in the CHD population, is reaching out and truly engaging all members involved in your infant’s care team that is rallying for successful growth and nutrition. This includes: first and foremost the family, pediatrician, referring and primary cardiologist, hospital teams (prenatally, postnatally in CICU, floor wards, and follow-up clinic visits), early intervention, speech/feeding therapy, and cardiac developmental centers available at your institution/region. These team players (from nursing, lactation, nutrition, MD, therapists, etc) along with family dedication are essential to ongoing success with breastfeeding for this high risk and fragile population - particularly during the interstage period. This period is often described as a very isolating experience for the family, particularly for a dedicated breastfeeding mother. Thoughtful discussions with mothers and families throughout all care opportunities with health care providers are critical to ensure the best outcome for the infant and family.
As Amy mentioned, breastfeeding and oral feeding in general is a lot of work and a "stress test,” particularly for infants with HLHS. Realizing this at baseline is important because there can be additional complicating morbidity factors that may impact the stress of feeding. Some of these concerns are: poor ventricular function, valve regurgitation, breathing fast due to too much blood flow or other respiratory concerns, vocal cord injury, oral aversion, reflux, other non-cardiac anomalies, and other morbidity factors that may contribute to an infant's failure to thrive and grow. Having said that, these factors should not limit the decision to utilize breast milk and all its beneficial immune properties.
Discussions with health care providers about breastfeeding and utilizing your precious breast milk is essential. It is also important to note, that there are some special cases such as chylous effusion (milky appearing fluid accumulating or draining around the lungs), milk protein allergy, or guiac positive (bloody) stools that may require alternative supports for nutrition. In these instances, a conversation about alternative options and adjustment in the breast milk diet may need to occur in the short term period.
Practical 5 Pearls of Wisdom to Share with Moms Interested in Breastfeeding
1. Discuss prenatally and postnatally your thoughts on breastfeeding. On a daily basis bring up your desire to encourage breastfeeding and connect with all your lactation resources early.
2. Keep your breast milk supply up drinking proper fluids and frequent pumping at least every 3 hours. If concerned, please reach out to your lactation consultant early. This way you will have plenty of that nutrient rich milk with all its beneficial immune properties when your baby is ready. *Please see below our lactation consultant expert from Boston Children’s Hospital, Karen Sussman-Karten’s input for other pearls of wisdom on breast milk supply and “lactoengineering.”
3. Practice patience and persistence. Never miss an opportunity to practice. Try to breastfeed or even just work on non-nutritive suck if your team agrees during the inpatient stay (preoperatively if possible) and outpatient. In some cases, you may need to be persistent in your requests to try breastfeeding, but don't be shy in speaking up for your baby. Once your child is on bolus feedings, there are at least 8 feeds at least in a day and thus 8 times to practice daily with the health care team and ultimately the primary feeders of the infant after discharge.
4. Advocate and utilize the resources available to you in the home surveillance monitoring program (saturations, heart rate, daily weights, and logging the number, volume, and length of feeds-particularly if breastfeeding).
It continues to be an issue among some institutions that insurances will not cover scales. Advocate early with your primary team, ask for scales that weigh to at least 10grams (there are many on the market), and if possible consider scales that weigh to <10 grams.
Communicate honestly with your providers about how the breastfeeding and growth is progressing. It is important to share with your providers if you are noticing fatigue, sweating or diaphoresis during feedings because these may be a sign that your baby is working too hard to feed to adequately grow and thrive.
Avoid feeding (by bottle or breast) longer than 20-30 minutes to minimize losing more calories during the feeding process than actually gaining. There are some weeks where you may need to add more bottle feeds due to your family circumstances or or infant’s illness. Make sure to pay particularly close attention to your baby’s progress with your home scale. These periods may warrant more detailed intake and should not be thought of as a failure to breastfeed successfully.
Remember the nature of shunt dependent blood flow in HLHS heightens your infant’s vulnerability during the interstage period, and this is the primary reason why home surveillance monitoring was introduced over a decade ago. In some cases, your infant may require to be seen by your local providers (cardiology or pediatrician) or visit the emergency room for reassessment of plan of care. Some instances may require readmission for closer monitoring of feeding and cardiovascular status. This is by no means a failure on your part, but the “nature of the disease process of HLHS.”
5. Be practical with your expectations. Don't expect your baby to fully breastfeed by the time of first discharge following stage 1 palliation (whether it is Norwood with BT shunt, Sano with right ventricular to pulmonary artery homograft, or Hybrid). Lastly, please remember that you are not alone, take care of yourself, and never give up!
Karen Sussman-Karten, RN, IBCLC
Karen is a Lactation Consultant in the Lactation Support Program at Boston Children’s Hospital and is currently the Board Chair of the Mother’s Milk Bank of New England.
Amy and Michelle have shared so much valuable wisdom about breastfeeding and providing breastmilk for CHD babies. I have been a lactation consultant at Boston Children’s Hospital since 2006 and I have a few more thoughts for you.
Having adequate milk production is the foundation for success. Without it your options are limited. Since your baby will probably not be able to breastfeed in the first few days, expressing milk is essential to establish milk production. It’s important to start as soon after delivery as possible. Pumping frequently, every 2-4 hours is recommended. You may be able to collect more milk with manual expression in those early days. “Hands on pumping,” massaging and compressing while using a breast pump, can also result in collecting more milk.
Think of your early breastfeeding attempts as practice sessions. Don’t expect your baby to drink large volumes at the breast initially. Try not to get discouraged; practicing will lead to improvement over time and the skin to skin contact can help with milk production and breastfeeding.
Once your baby seems to be drinking at the breast, doing a pre and post feed weight to measure intake can be helpful, particularly in the hospital when you have access to use a very accurate scale for pre and post weights. As mentioned by Amy, our parent expert, most baby scales intended for daily weight checks are not sensitive enough to weigh less than 10 grams. Of course purchasing an accurate scale can be costly. You may want to consider renting one like the Medela baby weigh scale for home based on your infant’s progression with breastfeeding. It’s very important to keep your baby in the same clothing and diaper for the pre and post weight. Changing the diaper or weighing your baby naked will not give accurate results.
“Lactoengineering” refers to ways of altering the breast milk or breastfeeding to meet your CHD baby’s specific needs. Since getting the most calories is a major concern, there are some techniques you can use to increase caloric intake. The caloric content of your breast milk can be tested using a creamatocrit machine or milk analyzer. Some hospitals have this equipment. The assumption is that breast milk has 20 calories per ounce but when tested it is often higher. This becomes important if your infant’s EBM is being fortified above 20 calories per ounce, potentially up to 26 or 28 or more calories per ounce. Some infants do not tolerate the additives for a higher calorie diet so it can be very helpful to know the general caloric density of your breast milk as a baseline. Sometimes the additives can be reduced or eliminated depending on the results. Beware, the fat content of your milk varies throughout the day so testing once is like a snapshot of the calories per ounce.
Another interesting phenomenon is that the fat content of your milk increases toward the end of a nursing or pumping session. If you make more milk than your baby drinks, you can use more of the fat rich “hindmilk” to increase the calories. You can pump for the first 3 minutes and freeze that “foremilk” for later use. Then either nurse your baby or pump the remainder of the “hindmilk” and use only that.
If your baby has a chylous effusion, they cannot tolerate the fat portion (long chain fatty acids) in breast milk. It is possible to separate the fat from your milk and use the “skimmed” breastmilk. This can be done with a centrifuge machine or with other methods of allowing the milk to separate and removing the cream layer. This “skimmed” breast milk will need to have other oils and nutrients added to make up for the calories lost by removing the cream. This allows your baby to continue receiving your milk rather than a special formula while they have a chylous effusion.
Thank you so much, Michelle and Karen for your helpful insights into breastfeeding a child with a complex congenital heart defect like HLHS!
Stay tuned for next week’s post in our nutrition series, “The Cardiac Newborn!”
Breastfeeding the HLHS Baby - the Parent Perspective
Nutrition Series
By: Amy Bennet, Parent
March is Nutrition month! In honor of Nutrition month, we’ve created a special blog series on nutrition. We’re kicking off the month with a post on breastfeeding, written by one of our own Sisters by Heart moms, Amy, mom to Bodie. We will follow it with a series on nutrition issues faced by our HLHSers, all provided by Emily LaRose, Dietitian at Children’s Hospital of Los Angeles. Without further adieu, Happy Nutrition Month – and happy breastfeeding!
“Will I be able to breastfeed my baby?” This question gets asked SO often, and the answer is not terribly straightforward. I wanted to take a few moments to answer this question from the perspective of a mom who’s been there and wondered the exact same thing.
I should mention that I’m a huge fan of breastfeeding. I breastfed my heart-healthy (now 5-year old) daughter until she self-weaned right around her 2nd birthday. So, breastfeeding is important to me. It was something I desperately wanted to do with my HLHSer, but, for a myriad of reasons, was unable to. I ultimately pumped for him for 10 months and had enough breast milk to last him until 15 months of age. For most HLHSers, breastfeeding, at least exclusively, simply isn’t feasible. There are a lot of factors working against breastfeeding our special kiddos. The rare mom who is able to exclusively breastfeed is a bit like an exotic animal observed in the wild, while the rest of us stare and whisper in awe. BUT it is possible for some mothers, and partially breastfeeding is possible for many more. If breastfeeding is important to you, by all means, try to make it work! Here are some things to keep in mind:
Monitoring
Many hospitals follow an interstage monitoring program, which requires parents to track specific data points (i.e. oxygen saturations, heart rate, weight, intake). Thus far, monitoring programs are reducing interstage mortality. Feedings are tracked closely interstage, since even slowing down slightly during feeds raises a red flag for practitioners. The ability to monitor the exact amount of “ins” for your baby is crucial – an easy task when armed with a bottle, but obviously more difficult with breastfeeding. For this reason, some hospitals discourage breastfeeding. Some doctors are uncomfortable with how difficult it is to measure feeds done via breastfeeding. But it’s not impossible! You can overcome this obstacle if your insurance approves a scale, by purchasing a baby scale, or renting one yourself weighing your baby before and after each feed to calculate the exact amount of breast milk taken. It’s more challenging, but definitely not impossible. There are some scales that weigh to smaller increments, but are also much more costly. Finding one that weighs to 10 grams is often reasonable enough for most families to track the daily weights.
Weight gain and cardiac function
This is probably the biggest obstacle to exclusively breastfeeding an HLHS baby. One of your primary goals interstage is to grow your HLHSer big enough to be ready for his or her second stage surgery, either the Glenn or the Hemi-Fontan. Many interstage HLHSers struggle with growth because their hearts are working so hard. It’s very common for interstage babies to receive supplemented formula or breast milk for higher caloric concentration. In my case, I pumped, and my son was not able to gain weight on the calories in my breast milk alone, so my pumped milk was fortified with a high calorie formula. If your baby cannot gain weight on the calories in breast milk alone and fortification is necessary, exclusive breastfeeding simply may not be a possibility, at least until after the second stage surgery when growth is typically less of an issue. But, that doesn’t mean you can’t breastfeed at all. I do know a number of HLHS mothers who’ve breastfed a few times a day and fed with fortified formula for the remainder of their feeds. If this is the only thing stopping you, definitely check with your cardiologist to see whether this might be a possibility.
Related to weight gain, it takes a lot of work to eat, whether by breast or bottle. For some babies, particularly those whose cardiac function is depressed, it can be really hard to gain enough weight on oral feeding, even if it’s supplemented, because their hearts are simply working too hard. For these babies, tube feeds are necessary to allow the baby to grow without having to work for it. But again, that doesn’t mean you can’t pump breast milk and tube feed your baby, so that they can still get the immune boosting benefits of breast milk.
Swallowing
Another thing that can sometimes play a major role in whether or not you’ll be able to feed is whether your baby has any swallowing issues. In my son’s case, his left vocal cord was paralyzed during his Norwood (not an uncommon complication following open heart surgery where work is done on the aorta, as the nerve controlling the vocal cords run alongside the aorta – due to the extensive amount of aortic reconstruction during the Norwood, this complication is seen). Vocal cords are what protect the baby’s airway. For a baby with vocal cord paresis, the paralyzed vocal cord lacks the ability to adequately protect the airway and, depending on the severity of the paralysis, oral feeds may need to be thickened using a thickening agent or avoided altogether. In either case, although breastfeeding is not safe for the baby until either the affected cord heals or the remaining cord compensates, you can still pump breast milk and feed it to your baby via bottle or feeding tube.
Feeding Difficulties
Many of our HLHSers have difficulties with feeding in general. Often, these difficulties come in the form of oral aversions, or difficulty coordinating sucking, swallowing and breathing simultaneously. There are many factors that can cause this. For babies at institutions that do not allow oral feeds prior to the Norwood, sometimes, by the time the baby has had surgery, been extubated and finally given a chance to take a bottle or breastfeed, the newborn’s sucking reflex is gone and they quite literally do not know what to do with a bottle or breast. Or they can suck, but can’t quite coordinate their swallowing and breathing effectively. For others, particularly those on the ventilator for prolonged periods of time, they may associate things being in their mouth with discomfort and pain, and oral feeds are quite challenging. In both of these cases, breastfeeding is unlikely; however, there are a few things you can do to try to work through this and enable your baby to take a bottle of pumped breast milk.
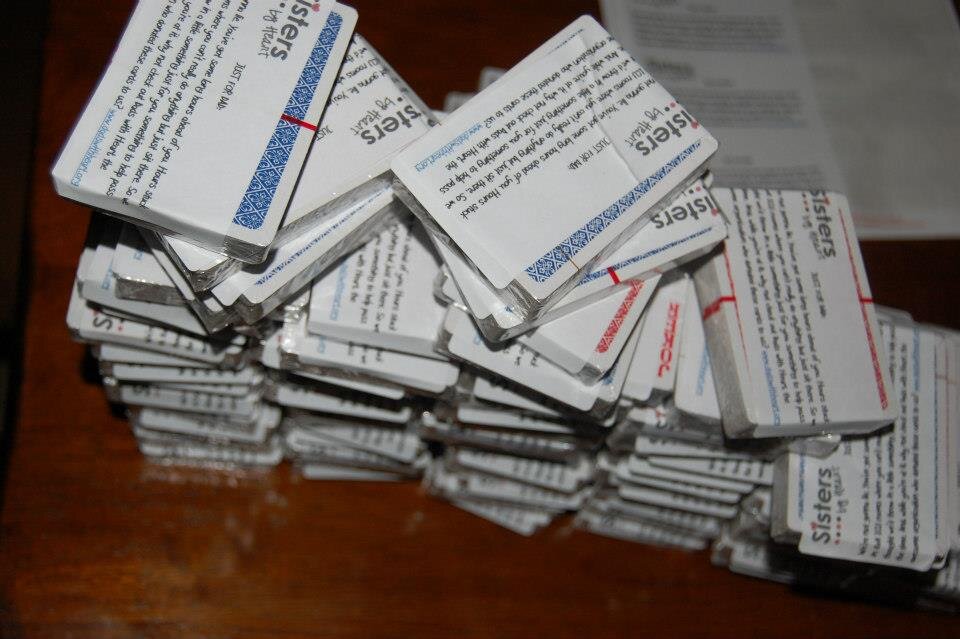
In Sisters by Heart care packages, we include newborn pacifiers, and encourage parents to use them with their newborn prior to surgery and until the baby is permitted to attempt oral feeds. While it will not guarantee a baby will retain that sucking reflex, it can help keep the baby in touch with that sucking reflex. You can also ask your medical team to intubate through the nose, rather than the mouth, so that the baby can take a pacifier even while intubated. (Some, but not all, institutions can comply with the request, depending on your child’s situation.) And, definitely, seek out occupational therapy, lactation specialists and feeding therapist as soon as possible at your surgical center because they are often very practical at providing a lot of strategies to encourage oral feeding and breastfeeding.
As you can see, the question of whether or not you’ll be able to breastfeed your HLHSer, or any complex CHDer for that matter, can be a loaded one, dependent on a lot of factors. Yes, the odds are stacked against you being able to exclusively breastfeed, but that doesn’t mean it can’t happen; many mothers are able to pump and alternate breastfeeds with bottle feeds. If this is something that’s important to you, then push for it. Let your medical team know upfront that you intend to breastfeed (I told my entire medical team while I was still pregnant, in fact!).
And if breastfeeding simply isn’t an option for any of the reasons mentioned above, pumping is almost always an option – so, to those of you moms who fall into this category, I say pump, pump and pump away!!! The benefits of breast milk are huge, regardless of the source: breast, bottle or feeding tube. It’s not easy to pump exclusively, but take it from someone who’s been there, in your shoes – it is absolutely worth it! Do what you can to keep your supply up and pump as long as you can – whether it’s 1 day, 1 week or 1 year, your CHDer will receive benefits!
Many hospitals have resources dedicated to lactation support for cardiac patients, so make sure to ask! For instance, Children’s Hospital of Philadelphia provides a lot of great information on breastfeeding a cardiac patient here!
Another hospital currently focusing on lactation support for cardiac patients is Boston Children’s Hospital. Stay tuned for Thursday’s post, where two practitioners from BCH share their input on this important topic!
Thank you, Amy, for sharing your insights with us!
Practitioner's Perspective: We Can't Make It All Better
Darci Walker, PsyD, Founder of Core Parenting
Parenting an HLHS child is, well, different. HLHS brings an entirely different set of parenting challenges and struggles. Sisters by Heart is grateful to Dr. Darci Walker who helps explain the struggles we may face, from a psychologist's perspective. Thank you, Dr. Walker, for lending your most insightful thoughts to our HLHS families.
This child. This parent. This moment.
I remember the moment I stepped outside of the hospital for the first time with my firstborn son. I remember a feeling of sheer terror. I looked at my husband, and he looked at me, and we looked at this little thing in between us, and one of us actually said, “Really? They are just going to let us walk out of here with him? What the hell do we do now?”
The enormity of the future weighed so heavily in that moment. My job seemed impossible. I was unprepared and unqualified and unsuspecting. I needed to protect him. Keep him safe. Keep him healthy. Make sure that the world is safe and secure and he has all the goodness he deserves.
I knew, in that moment, that I was completely incapable of actually ensuring that his road would be completely smooth and that nothing bad would ever happen to him. And that realization hit me like a ton of bricks.
But, I was lucky. He was healthy and I was able to seek comfort in the fact that I could worry about impending doom another day. Right then, he was okay. I could breathe and let myself believe that I had more control than I really did. I would have some time to figure out what parenting is really all about. I could wrap myself in a delusion of control. Like the myth that my very kiss could make an owie disappear. And, somehow, that myth helped me through the early stages of parenthood.
Of course eventually, for me as for all parents, the myth would shatter, and the true depth and challenge of what parenting really is would become clear. For many parents it’s the first time your child gets hurt. Or bleeds. Or has an incredibly high fever. Or gets lost. Or gets bullied by someone. This is when some parents really figure it out, when the real truth of parenting sinks in. The powerlessness of it all. The truth that this little human, that came out of our bodies, is really on their own path. We are not in control of their lives and we can’t protect them from all things. No, our job is not to kiss away the owie. Our job is to be with them, no matter how painful the owie. Parenting is about walking impossible paths and tolerating impossible pain and supporting our kids through impossible limits. It’s not about making it go away. Because we can’t. It’s not about making bad things not happen. Because we can’t always do that either. It’s about being by their side. This child. This parent. This moment.
It’s in these moments of utter pain that we realize that all we can do is do the best we can to stay beside them and love them and give them every ounce we have, but in the end, every ounce won’t really be enough to eliminate all pain and suffering. And while this is really true for all children from day one, many of us don’t have to learn the agony of that realization for some time.
But, other parents have to hit the ground running. Parents who have babies born prematurely or who have babies with medical issues, like children born with hypoplastic left heart syndrome, never have a chance to feel this calm before the storm. Parents who have babies that move from the delivery room to the NICU faster than a blink of an eye never have a chance to wrap themselves in a false sense of control and comfort that they can make everything all right.
Right from the start, these families are forced to watch from the backseat as their little person travels on their own path, surrounded by doctors and machines and tubes and acute needs. Right from the start these parents have to live with the truth that they can’t make it all better. That their kiss doesn’t really make the owie go away. And that realization is heart wrenching. There is so much anxiety, fear, depression.
These little people have a tremendously difficult road ahead of them. Their families have enormous pain to endure. And yet, there remains: This child. This parent. This moment.
If we can let go of our myths about what parenting means. If we can let go of our fears about the future. Just for a moment. Then we can realize that what this child, what any child, needs in this moment is a parent who can tolerate the pain and be there with them. By their side. Walking this path, this painfully difficult path. Holding them, rocking them, touching them, fighting for them, singing to them, smiling at them, crying with them, reading to them. That is parenting. This is parenting. This moment of connection and support and touch is parenting.
I worked with a family whose infant son died hours after birth. While they knew that their son would die soon, they knew they had a very important role in his life. They held him, they rocked him, they sang to him. They talked to him and whispered in his ear and cried with him as he died. This is parenting. This child. This parent. This moment.
I can’t claim to understand the enormity of having a sick child. But I do know the difficulty of letting go of my expectations, my feelings that I have somehow failed my child, my feelings of frustration with a world that is unfair and harsh and cruel. I do know the pain of watching a child struggle with something that I can’t un-do. And I do know that sometimes, when all I want to do is crawl into my bed and hide from it all, what I need to do instead is just go be there with my child.
And I also know how amazing it feels when I can truly be there in the moment for my child. This child. This parent. This moment.
My child and me. Now. Touch, hold, connect, support.
That is parenting. I do know that the feeling of connection and strength and beauty that comes out of it is the most important thing in both our lives. Because while the kiss can’t make the owie go away, the connection in that kiss can give the child the support he needs to know that he can take the next step. What a gift. Parenting in its most pure and true sense.
Dr. Darci Walker, is a mom to two boys and Clinical Psychologist with experience working with families, individuals and children in a variety of settings. In 2010 she co-founded Core Parenting in Portland, Oregon and specializes in working with parents and the variety of transitions that occur during this amazing stage of life. From postpartum depression to relationship difficulties, career changes to identity reformation, Dr. Walker is interested in the multiple layers of challenges and joys that parenting brings and loves working with both men and women as they negotiate through these processes, highlighting her belief that thriving parents lead to thriving children! Read more at Dr. Walker's Blog and on Facebook.
It's February, Celebrate Black History Month!
We know what you're thinking... Black History Month?! It's Congenital Heart Defect Awareness Week, why are you talking about Black History Month?! Well, the answer is simple - because of this brilliant man.
Vivien Theodore Thomas
(August 29, 1910 - November 26, 1985)
Vivien Thomas, the grandson of a slave, was an African-American surgical technician who developed the procedure we all know so well, the Blalock-Taussig Shunt or BT Shunt. Assistant to cardiac surgeon, Alfred Blalock, Vivien performed experiemental surgeries in the animal labratory at Vanderbilt University and Johns Hopkins University.
Thomas created Tetrology of Fallot in canines and then worked at correcting the condition by a pulmonary-to-subclavian anastomosis. The first dog to survive long-term was Anna - whose portrait was hung on the walls of Johns Hopkins. During Dr. Blalock's first BT shunt palliation, on an infant patient, Vivien Thomas stood on a step stool behind Dr. Blalock walking him through each step of the surgery.
With only a high school education, Vivien Thomas suffered through poverty and racism to become a cardiac surgery pioneer and ultimately a teacher of cardiac operative techinque.
In addition to the BT Shunt, Vivien pioneered surgical techniques improving circulation in patients with Transposition of the Great Arteries and the atrial septectomy (also performed for HLHS infants). Vivien's atrial septectomy was so flawless, Dr. Blalock exclaimed in the OR, "Vivien, this looks like something the Lord made."
If you haven't seen the HBO film, Something the Lord Made, we highly recommend it for Heart Awareness Month (or anytime really)! Enter to win a copy of it here!
Vivien Thomas was the first African American without a doctorate to perform open heart surgery on a white patient in the United States. We could go on and on about the life of Vivien Thomas; we owe so much to this man and his contribution to the advancement in HLHS palliative care.
If you want to read more about Vivien Thomas, you might want to grab his autobiography, which he began writing just a few years before he lost his battle with pancreatic cancer. In fact, Partners of the Heart was published two days after his passing.
A Unique Collaboration: SBH and the NPC-QIC
What a special day! Today...February 1, the official "Go Red" Day when we are all wearing Red to honor those affected by Heart Disease and Congenital Heart Defects, Sisters by Heart thought it was particularly fitting to announce a very special joint project we've been working on with the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC)!
Several months ago, Sisters by Heart began discussions with the NPC-QIC team about developing a video for HLHS parents, to be viewed prior to discharge from the Norwood, to set their expectations for the interstage period (between the Norwood and Glenn/Hemi) and give them reassurances that they were not alone during that terrifying time. Sisters by Heart took on the project with so much excitement, knowing that we'd have loved to have had something like that when we were discharged with our special babes!
We kept things under wraps, "secretly" doing our filming while on our annual retreat in September...
The NPC-QIC premiered the film at its Learning Session last weekend - and officially "went public" with it today, posting it to their page.
The hope is that this will be a useful tool for members of the Collaborative to use in their discharge planning, to better prepare parents for the interstage period. And, for families at hospitals not in the Collaborative (or in hospitals that are in the Collaborative but who aren't using the video in their discharge process), it will be available on the NPC-QIC's website.
Please go here to find out more about the Collaborative and how parents can become involved!
If you missed our blog post highlighting the Learning Session we attended last weekend, you can read it here.
We were so excited for the opportunity to collaborate in the creation and filming of this video and are proud to be able to finally show it to our families! Please share this and spread the word! Newly discharged families are not alone!
NPC-QIC Winter Learning Session
This past weekend, several members of our Sisters by Heart Board had the honor of attending the winter Learning Session for the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) in Cincinnati, Ohio. Over 40 pediatric heart centers sent representatives from their teams to share and learn from one another in an effort to continue improving the quality of care for HLHS babies between the first and second stage surgeries. Some of the top pediatric cardiologists, and their teams, were in attendance and it was truly an amazing experience to hear their passion for not just saving HLHS babies, but really improving the quality of their lives. The passion and determination exhibited by those in attendance was an inspiring, eye-opening experience; caring for HLHS babies is more than just a job to them. These physicians and team members genuinely care for our special kids and are working together to continue to improve their outcomes.
The Learning Session consisted of two days of intense discussions, speakers presenting information about their current home monitoring programs and inpatient treatment plans and breakout sessions centered around different subjects ranging from partnering with parents to developing ways to pre-plan appointments and actively engage pediatricians as care team members.
Amy, Natasha, Stacey, Stacie and Kathy
The NPC-QIC is currently focused on improving the mortality rate of HLHS infants during the interstage period. Some of their top priorities include improving growth by effectively treating feeding problems, and understanding and preventing readmissions to the hospital during interstage. The implementation of home monitoring programs has proven to be an instrumental tool in managing care for an HLHS interstage baby. Cardiologists are able to closely monitor the progress, or lack of progress, their patients are making by the information parents are recording at home. Parents are armed with interstage equipment (charts, scales, pulse ox machines), information, and emergency plans needed to catch any potential problems at home. Some centers even have Single-Ventricle Clinics, solely dedicated to managing their patients' care between the first and second stage surgeries.
In addition to the physicians and care team members, 15 parents from across the country were in attendance to lend personal experience. Parents were not only invited to attend the conference, but encouraged to participate in discussions, ask questions and answer questions presented by the care teams. Our voices, as parents, matter. Our suggestions are taken to heart and our opinions are evolving the established standards. It was incredible to sit amongst these cardiology teams from across the country and see firsthand their eagerness to ask question after question to understand the parental point of view.
Attending the Learning Session was such an incredible experience and we are thrilled to have the opportunity to be involved in their mission. We all left feeling inspired by the passion that permeated throughout that conference room. Speaking of inspiration ...a couple of us had a chance to meet Meg Roswick, a 21-year old HLHSer, who is truly living her life to the fullest. She and her mom, Patty, are like celebrities in the HLHS community. Such an inspiration to us parents! Some of us are told after diagnosis that our HLHSers will never be able to play sports. Patty raised Meg to not let her HLHS define her and let her live like a "normal" kid. Meg found her passion for gymnastics when she was just a toddler and now she is a competitive gymnast who loves extreme sports and is even training for a half-marathon! She's in college and studying bio genetics. Meg and Patty are both amazing and give us so much HOPE for the future of our kids. Thank you Meg and Patty for coming out to meet us and continuing to inspire heart parents across the country by sharing your journey and opening your hearts to us!
Stacie, Stacey, Meg & Patty
It is obvious from our experiences this weekend that working as a team (cardios, nurses, pediatricians, dietitians parents, etc.) can greatly improve the challenging interstage period. The feedback parents received from the cardiac teams following the Learning Session was extremely encouraging and uplifting. We're look forward to participating in the next NPC-QIC learning session, scheduled for September 27 and 28, 2013 to continue with this mission.
If you're a parent or caregiver of an HLHS child, or child requiring the Norwood and Glenn/Hemi, and would like to become involved in the cardiology improvement collaborative, please visit https://jcchdqi.org/ for more information.
To follow in Meg's journey and learn more about her, feel free to visit her Facebook Page!
* No donations or Sisters by Heart funds were used for attendees travel expenses.
A Heartfelt Donation: Smart Mom Jewelry
Sisters by Heart loves to hear about products that help BOTH our special heart babies and their amazing mothers. We're even more excited when we are able to include these products in our care packages. So, you can imagine we were over-the-moon when we were approached about a donation of "Teething Bling," beautiful teething necklaces created by Smart Mom Jewelry.
Teething Bling® is the original teething jewelry, made from the same FDA-approved material as most teething toys. The pendants and bangles look great on mom and are safe for curious babies to handle and chew.
For the month of March 2013, Sisters by Heart is teaming up with Smart Mom to raise awarness for Congenital Heart Defects and would love to hear your CHD story. Please share your story with us at info@smartmomjewelry.com for a chance to win the beautiful heart pendant shown below!
A big thanks to our fellow heart mom Jackie, mom to this adorable CHDer, Zoey...
..who approached Smart Mom Jewelry about CHD and pulse oximetry awareness...and came away with an incredible donation of these beautiful teething necklaces for our care packages!
Amy Creel, founder of Smart Mom Jewelry, is committed to continuing to support and donate to Sisters by Heart! We are absolutely blown away and know our moms will be as well!
Like so many of our donors, Amy's reasons for donating are very personal. The loss of her sister-in-law, Maria, ignites her ongoing passion to give back to others. Amy's allowed us to share Maria's story with you...
"My sister-in-law - Maria Jankowski Maurer - died suddenly in 2006 of an undiagnosed and untreated CHD.
Maria was an accomplished artist and designer at Eileen Fisher. Because of her love of fashion and interest in women's issues, Smart Mom Jewelry supports great causes like Dress for Success in her memory. The mission of Dress for Success is to promote the economic independence of disadvantaged women by providing professional attire, a network of support and the career development tools to help women thrive in work and in life. We hope it is a fitting tribute."
We're pleased to be yet another organization that Amy is inspired by - through the many moms and infants we serve on a daily basis.
Thank you so much Jackie, Amy and Smart Mom Jewelry for your generosity in partnering with us to spread the gift of HOPE to newly diagnosed HLHS families!
Heartfelt Donations: aden + anais and The Dorsett Family
Our heart community has suffered more devastating losses this year. It's heart-wrenching to watch a fellow HLHS family say goodbye to their little warrior. With each loss, we are painfully reminded of the battle our children are fighting every single day. Each of our angel warriors holds a special place in our broken hearts. It's tragic and unfair that they can no longer be here on this earth with us and in the arms of their Mothers.
One of our HLHS warriors, Hayden Jeter Dorsett, earned his angel wings at just 5 months old. This sweet, beautiful baby boy with his big blue eyes, an infectious smile and adorable red hair would brighten our day when his Mom, Ady, would post precious pictures of him. You couldn't help but fall in love with the Dorsett family. When the news of his loss spread throughout our heart community, we all sobbed uncontrollably as we do every time we lose one of our own. The Dorsett family received an outpouring of support from family, friends, the heart community and even complete strangers. Thousands of people were touched by sweet Hayden in his short life.
Ady contacted Sisters by Heart shortly after his passing to offer a special product donation for our care packages in honor of Hayden. The nurses who cared for Hayden oohed and ahhed over him and the gorgeous aden + anais Swaddle Blankets he was always wrapped in. Hayden quickly became known for these blankets and it was rare to not see him swaddled in or sleeping soundly on one. Swaddling is extra comforting to our heart babies because we can't always hold them. Wires, tubes and med lines prevent us from snuggling our babies far too often in those first few weeks of life. Ady wanted the babies receiving SBH care packages to have their very own assortment of aden + anais Swaddle Blankets. She contacted them directly to see if they would allow her to purchase wholesale. Astonishingly, aden + anais responded saying they were so touched by Hayden that they would donate 104 (4)pks of swaddle blankets! Along with Ady, they also loved the idea of having our newborns wrapped in the comfort of their swaddle blankets in honor of sweet Hayden. More amazing yet, the Dorsetts offered to provide the aden + anais blankets after the donated supply runs out to continue honoring Hayden by helping as many families as possible.
Not only is baby Hayden watching over our heart warriors, he is now keeping them safe and comforted when they can't be in their parents' arms, neatly tucked into an aden + anais Swaddle Blanket and embraced in a sweet angel hug from Hayden.
"Angels are the guardians of hope and wonder, the keepers of magic and dreams." ~Unknown
Thank you aden + anais for your extremely generous donation of swaddle blankets in memory of Hayden. What a beautiful contribution to our care packages. We are truly grateful and honored to be able to provide these blankets to our newly diagnosed families.
And thank you Ady & Rob Doresett for your support to Sisters by Heart and sharing Hayden's journey with us. Hayden will always be a part of our SBH family and be forever missed. His memory will live on in our hearts and his life will continue to be celebrated through our care packages. Sending much love to you, Rob and Jackson today and always.
If you are as touched as we by the generosity and kindness of aden + anais, or are interested in their products, you can check out their full line on their website or send them some love on their Facebook page. They also offer some helpful tips here on how to help your newborn get a good night's sleep.
To read Hayden's story, or send the Dorsetts some love and prayers, you can visit Hayden's blog or Prayer Page for Baby Hayden on Facebook.
Want to share a picture of your newborn in a aden + anais swaddle blanket, or using other much-loved care package items? We would love to see them! Feel free to post on our Facebook wall or send via email to: info@sistersbyheart.org.
Gifts from the Heart: Stella & Dot
Sisters by Heart is thrilled to announce a wonderful opportunity to jump-start your holiday shopping, support our mission and celebrate our Second Anniversary - all at the same time!
Sisters by Heart teamed with Diane Gates, RN in the Cardiac ICU at Seattle Children’s Hospital and Independent Stylist for Stella & Dot, after Diane inquired about hosting a trunk show to benefit our mission. In addition to donating 100% of her proceeds from the LOVE and COURAGE bracelets to SBH, Diane opened up her entire online trunk collection, offering SBH 50% of the proceeds from those sales as well! Diane's trunk show sale is available today through December 5th. You can access the sale here!
If you'd like to purchase one for yourself or are searching for a great holiday gift for family, friends, your favorite cardiac nurse, cardiologist or therapist, now is a great time to do so! We've made special gift tags if you're giving the LOVE or COURAGE bracelets, so feel free to download the PDF below (open in a new window to print it) to include in your gift to show the thoughtfulness this gift brings.
And, of course, we asked Diane to share some of her story and her inspiration with us...
This is a privilege for me.
As an ICU nurse in the Cardiac Intensive Care unit, taking care of families whose children have been diagnosed with HLHS has been part of my life. I have been with many families over the years during the ups, the downs, the struggles, the victories, the laughter and the tears.
About 10 months ago, I also became a Stella & Dot stylist. Having never really been into jewelry before, I found myself pretty smitten with it. It’s beautiful. But more than anything, I became a stylist because I am a ‘connector’ by nature and I found that the company and the jewelry connected more than the links of its pieces… it connected people.
I don’t think it was totally by chance that I met Sara Hale (an SBH Board member) at one of the jewelry parties. As she shared some of her experiences with her own son, Townsend, and her passion for her organization, Sisters By Heart, I immediately sensed an opportunity to make a difference for something that as a nurse was close to my heart as well. Sara and I emailed back and forth as we figured out the details. We chose the Love and Courage bracelets because it is exactly that, love and courage, that is the essence of every family's journey.
Now through December 5th, I will be donating 100% of my commissions for these two bracelets to Sisters by Heart. In addition, I will be donating 50% of my commissions for any of the other items ordered. All orders will be received in time for the holiday season!
Thank you very much in advance for your support. It is my hope that when you, your friends or your family members wear these bracelets, that you feel the connection to this very special cause.
~ Thank you so much Diane, for your heart, your dedication to our families and for your generosity to Sisters by Heart!
Note: the bracelets are currently on back order; however, our wonderful Stella & Dot rep assures us that they will ship on 11/30 and arrive to you in plenty of time for Christmas!
Creative Donors: United Way Workplace Campaigns
Sisters by Heart sent out 100 care packages in its first year. We doubled that during the following 9 months, and are on track to send out over 300 next year! There is no doubt that there are a lot of families in desperate need of the HOPE that Sisters by Heart provides. Our growth has been astounding. Along with growth comes new challenges; mainly, how to fund that growth. So you could say that fundraising is at the forefront of all of our minds right now!
One of the easiest and most effective ways we've been able to raise funds is through Workplace Campaigns. Workplace Campaigns are fantastic, because they allow an employee to have a small amount withdrawn from their paychecks; the amount is small enough the employee hardly notices the reduction in income, but it can add up to a sizeable donation to a charity over the course of a year. And the contribution is completely tax deductible to the employee.
Did you know that you can contribute to Sisters by Heart through the United Way? Many employers do United Way Workplace Campaigns, and almost all United Way Chapters allow you to designate your funding for any 501(c)(3) who meets basic criteria (the criteria varies from chapter to chapter, but Sisters by Heart has met every criteria we've seen thus far).
If your employer does a Workplace Campaign that allows for designated funds (most do - sometimes you have to ask, but there's typically a space for it right on the form!), you can have a payroll deduction made to United Way and you can designate it for Sisters by Heart! On your enrollment form, simply list 'Sisters by Heart' and the contact information requested.
(The forms vary from chapter to chapter - this is from the United Way of Greater Los Angeles.)
Yes, it's THAT easy. We had two donors contribute that way last year and already have one signed up for next year! We know this is the time of year United Way forms are due for Workplace Campaigns, so if your employer participates, please ask about contributing to Sisters by Heart!
Even better, ask whether your employer matches! Many do! This is such a simple way to give the gift of HOPE to so many families!
If you have any questions or would like to find out more about the UW Workplace campaign, please contact our Secretary/Treasurer, Amy Bennett, at amy@sistersbyheart.org.
A Mother's Perspective: Healing a Hurting Marriage
Any parent who has a medically fragile child will tell you that it can (and often is) challenging to all relationships in your life, but perhaps most especially, your relationship with your mate. One of our Board members blogged about this subject recently, and received quite a response from members of the heart community. Her writing is insightful and we wanted to share it here. This is the first writing in the series. You can see the rest of the series at www.hopeforbabybennett.com. Thank you, Amy, for sharing your story with us!
Hope for Baby Bennett: Healing a Hurting Marriage: Part 1. The Backstory
Having a medically fragile child, particularly with a diagnosis like Hypoplastic Left Heart Syndrome, involving multiple open heart surgeries, can put an unbelievable amount of stress on a marriage. Before your diagnosis, it’s like your life is a nice tiny little ball of neatness (for the most part). Then, you get your diagnosis and the ball gets thrown in the air and completely explodes. Then, until your baby is born and for the first 6 months to a year of your child’s life (sometimes longer, depending on your child’s complications), you’re trying like mad to keep the pieces in the air as much as you can. You’re trying to keep things from hitting the ground. And you’re so busy trying to keep the important pieces (you know, keeping your kid alive) up in the air, you’re pretty much ignoring the unimportant ones. You’re making spur of the moment decisions on what’s unimportant enough to hit the ground.
Then, once things settle down, and you’re far enough past the Glenn that the surgical experience starts to fade and the Fontan seems light years away, you finally have some time to look around and examine all of the pieces of your formerly tidy little ball of a life. Some pieces are bent, some are broken, some are just flat out missing. Where’d they go? God only knows – you were too busy juggling the other pieces to notice. And you try to scoop everything up into that tidy little ball again, desperate for order amidst the chaos. This is what I lovingly refer to as “post-Glenn Fallout” period.
You have to spend time getting to know this new life, this new “normal.” Maybe you allow yourself to process the grief – maybe you don’t. After all, your child is thriving, so what right do you have to feel any sense of grief? In so many ways, this life is SO MUCH better than the life you had expected. But it’s still different. And you can’t ignore the ways it’s different. And, as tempting as it is, you can’t ignore its effect on your marriage or relationship.
When we were first diagnosed, we met another family whose little boy was gearing up for his Fontan. They were such a loving family – the mom and dad were both so supportive of their sweet little boy. But my mom told me later that the dad pulled her aside and said his biggest advice was NOT to ignore our marriage during that first year of our baby’s life, that it could have devastating consequences, that that was his one big regret. His son survived the Fontan with flying colors. Their marriage did not. And they are just one story. So many, many families have similar stories to tell.
So, when we realized that we were allowing ourselves to drift complacently through this “Post-Glenn Fallout” period, and we were pulling apart instead of together, remembering that family, and so many others like them, we sought out a pastoral counselor, a trusted and loving confidant who knew us, and our family. Someone who could help us navigate through this next stage in life, and pull back together into a cohesive unit.
It has been amazing. One of the best decisions we’ve made. We’re already making such good progress – toward one another, for the first time in years, instead of away. What a wonderful relief.
One of the first “assignments” from him was to write Bodie’s story. We looked at one another and said “sure, we have his medical history already written up.” He stopped us and said “No, I don’t want BODIE’S story. I want to hear how Bodie’s story has affected AMY. And how Bodie’s story has affected DUSK.” Interesting. He also asked us to write about what we’ve learned and about our celebrations and accomplishments. We talked a lot about celebrating milestones. And I realized that although we have been very good at celebrating how far BODIE has come in this journey, we have NOT been very good at celebrating how far the REST OF US have come – Dusk, me, Sierra, our marriage, and our family.
We protested a bit – it feels weird to celebrate how far we’ve come when we still have so far to go. Wouldn’t we be somehow jinxing things? But he gently reminded me that, much like soldiers at war, just because we know we have another tour of duty coming up does NOT mean we don’t celebrate each homecoming from a tour. So, in the next few blogposts, I will be sharing both Dusk and my writings of celebration, and our trip this last weekend, our first weekend away together since before Sierra was born!
A Gift for Our Fighters
We call our heart kiddos fighters, warriors, heroes, HLHS butt-kickers...because they are the strongest, bravest, most-determined people we know. From the moment they are born, they begin fighting a battle that we ourselves, as adults, would find nearly impossible to face. For us, their battle begins the day we receive the devastating diagnosis. We become strong for them and continue to fight with hope in our hearts for their future.
Our kids are inspiring and continue to amaze us every single day. Our lives are forever changed by their heart journeys. We see the world differently and appreciate every single minute we have with them. We love to share their stories because we are SO proud of them for everything they have endured in their first few months and years of life. Their half hearts make our families whole and we love them unconditionally.
I (Stacie Jackley) recently had the opportunity to honor my little figher, Kellen, with a song written and fully produced for him appropriately titled "Half a Heart." My cousin, Tyler, is a multi-talented musician & professional recording artist and a member of Gym Class Heroes since 2005. He plays the keyboard, guitar, does backup vocals and wrote many of their songs - an incredibly talented kid.
Tyler is the second from the left
When I first heard this song, I sat there stunned with tears streaming down my face. It's not just about Kellen, it's about all of our HLHSers. Their fight, the pain, the hope... In listening to the lyrics, you would think Tyler is the father of a heart child. It's so beautifully written and heartfelt. I wanted to share this song with all of you, as a gift for your HLHSers. I truly hope you enjoy it as much as I do.
Thank you Tyler for sharing your talents with us and giving Kellen and his friends such a priceless gift that we can cherish forever! You are amazing.
Want a chance to have your own personalized song for your HLHSer? Enter our 2nd Annual SBH Costume contest! We will be accepting entries until 11/4. The album will be posted on 11/5 and the voting will begin! The Halloween cutie with the most "likes" will win their own song written and produced by Tyler! How cool is that?!
A Practitioner's Perspective: Choosing a Pediatrician/Vaccinating your HLHSer
By: Jennifer Melnychuk, MD ("Dr. Jen"), All Star Pediatrics Exton, PA
To introduce myself, I am a pediatrician in private practice in the Philadelphia suburbs. I have been in private practice for over six years. Prior to that, I completed my residency training at the Children’s Hospital of Philadelphia. My experience with children with congenital heart disease has come from both caring for patients in the hospital as well as in the out-patient setting.
Awaiting the arrival of a new baby is such an exciting and scary time for any family but even more so for parents of children with heart disease. Not only do you have to research a pediatrician for your newborn, but you have to select a cardiologist, cardiac surgeon, birth hospital, etc. It only made sense that the Sisters by Heart website wanted to offer expecting parents some advice when selecting a pediatrician and I was so pleased when they asked me to weigh in.
While you will be spending a lot of time with the cardiology staff, your general pediatrician will also play an important role in your child’s care. Your pediatrician should be familiar with complex congenital heart disease from diagnosis to post-op care to long-term follow-up. You should ask where your pediatrician trained, as certain medical centers specialize in cardiac care. He or she should be board-certified in pediatrics which means they trained at an accredited pediatrics program, passed the board exam and maintain educational requirements and quality improvement projects. In a busy pediatric office, your pediatrician should allow extra time for your child’s visit, including special attention that should be paid to growth and development. You will have lots of questions (and you should never be afraid to ask a question!) and you want to make sure your doctor has the time to answer them all. Your doctor should also stay updated on your child’s specialty care and have a contact through the medical center to remain informed.
Finally, you should ask how you can contact your pediatrician as concerns arise both when the office is open and after-hours. Your pediatrician should respond to your questions the same day and you should be familiar with the other providers (and they should be familiar with your child’s care) in the practice for when your pediatrician is not in the office. You should have easy access to a physician after-hours as well for emergencies.
The rest of the staff including the front desk staff, the nurses and the billers all play a role in your child’s care as well. The front desk staff should be aware that your child has complex needs - they may schedule appointments when the office is less busy or have your child brought back to an exam room immediately so your child is exposed to less illness in the waiting room.
The nursing staff who are answering questions on the phones during office hours should also know that your child has heart disease. For example, the nurses may give different advice about a cough or a fever for a patient with complex medical needs. The nurses should be knowledgeable about your child’s medications as they will often be refilling them. Your child likely will need many referrals for specialty care which the nurses or a referral coordinator will help you with.
The billing staff will be crucial to help you navigate insurance issues as they arise. Certain states provide supplemental insurance for children with complex health needs and your pediatrician’s office should be familiar with those options and accept those insurances.
My final thoughts involve the importance of vaccination for all children, but especially those with chronic medical conditions. Children with heart disease are particularly vulnerable to complications of many illnesses and we need to protect them as much as possible.
Illnesses that attack your child’s lungs require special attention for children with heart disease. While influenza (“the flu”) may just cause fevers, body aches, and a lingering cough in some children, a child with heart disease could end up in the intensive care unit from the same illness. Your pediatrician’s office should have a system in place to prioritize your child (and his or her siblings) to receive the flu vaccine as soon as it becomes available.
Respiratory Syncytial Virus (or RSV) can also be devastating to certain groups of children like those with heart disease or infants that were born premature. Unfortunately, no vaccine provides long-term immunity against this illness. Children who are at highest risk are recommended to receive monthly injections of antibodies to protect against this illness during the peak season – typically from October to early Spring. Again, your pediatrician’s office should coordinate this for you. Please make sure you have a contact person in the office to assist in insurance coverage for this very expensive immunization and to assist in setting up your monthly visits to receive the injection.
You have probably heard that pertussis (or whooping cough) has been making a comeback recently. This past year has seen a significant rise in the number of cases due to a number of factors including groups of families who chose not to immunize their children and adults losing the protection of the vaccines they received as children. Please make sure your pediatrician is up-to-date on the latest recommendations on immunizations from the American Academy of Pediatrics, as changes can come up.
Please also insure that any person that has frequent contact with your child also has received his or her vaccines – like the flu and whooping cough (Tdap or DTap) – including you, grandparents, daycare providers and even the staff that works at your pediatrician’s office. It is also wise to ask about your pediatrician’s office policy on vaccination. Recently, more offices are asking families that chose not to vaccinate their children to find another provider. This is primarily to protect other children in the office. While no vaccine provides 100% protection, you want to assure that the other patients in the waiting room are fully vaccinated so diseases like the flu, whooping cough, and measles are not spread by visiting your doctor.
While there is so much to think about, always remember your child is a blessing and will provide you with countless joy. Good luck!
Jennifer Melnychuk, MD ("Dr. Jen")
All Star Pediatrics
Thank you Dr. Jen for sharing your experience in treating complex cardiac patients and offering your insights into caring for them. We, at Sisters by Heart, greatly appreciate your time and contribution to educating our HLHS families on the importance of vaccinations and guidance on choosing the right Pediatrician for their child. We know our families will be equally as appreciative for your time and expertise!
Helpful Tip: Most Pediatric offices will allow expecting parents to set up an appointment with one of their Pediatricians to give them an opportunity to ask questions and find out more about the practice. Here is a list of questions from the JCCHD Parent Page (suggested by HLHS parents) you can ask when meeting with a Pediatrician. As Dr. Jen mentioned above, your child's Pediatrician is an integral part of his or her care team - it's important that the docs and office staff accommodate your needs, especially during interstage. If they are not willing to do so, you may want to keep looking!
Stories of Hope: Tyler Sajdak
Meet Ty - All Boy, All Sport
Hello, my name is Tyler Sajdak. I was born with the congenital heart defect Hypoplastic Left Heart Syndrome in Grand Rapids, MI on September 18 of 1993. Six days after I was born I was taken to Ann Arbor, MI, for my first of three open-heart surgeries. Dr. Edward Bove was the surgeon who performed my surgeries at the University of Michigan hospitals.
I grew up feeling like a normal kid. My parents, as best they could, treated my siblings and I as evenly as they could. They never wanted me to feel like I was more or less special then my siblings were. My dad, his brothers and my older brother got me into sports, especially baseball, at a really early age. My uncle gave all of my siblings ping-pong balls when we were little so we could throw them and get used to holding a ball, something my two brothers and I did frequently. When we were little, we would always either be outside throwing a baseball or football or trying to beat each other in sports video games.
During my early elementary years, I started playing organized sports. I played rec league baseball and soccer while I lived in Orange City, IA, and I started play little league baseball and rec league flag football when I moved to Pella, IA. I always felt like I was one of the better players on both the baseball diamond and football field. I played shortstop and pitcher in little league, and I even threw a no-hitter. In flag football, I played quarterback on offense, and I tried to get my coach to let me play middle linebacker on defense, but I rarely played defense because “you don’t want to get your quarterback hurt”. During my 6th grade flag football season I led my team to an undefeated season, 6-0.
During middle school I stopped playing organized football and joined the school soccer team instead. I was the goalkeeper on my 7th and 8th grade teams. That is when I started to like soccer as a pro sport. I am an avid Chelsea FC fan because of my two years as a goalkeeper in middle school.
I started playing high school baseball my 8th grade year. That is when I moved to catcher. I absolutely loved playing catcher. I think it is a great position for anyone with HLHS to play. It doesn’t involve that much running and you are in on every single play. I only played until my sophomore year, but it is still my favorite sport to play.
I took up tennis when I started high school. My older brother was a senior on the tennis team when I started playing. He was the reason I started playing tennis. My dad had convinced my older brother to play tennis, and in the process convinced me to play too.
Now that I am in college, I haven’t had that much time to continue playing sports. I will toss around a football with some of my friends every now and then, but I didn’t join any of the school’s sports teams. I am planning on joining a slow pitch softball team in the spring just to keep my energy level and my love of sports “up to date."
I hope this has helped all of you. If you have any other questions you would like to ask me about my experiences in sports or any other sphere of life. don’t hesitate to ask.
Thank you Ty, for sharing your journey and experiences as a young boy growing into adulthood. Many of us, at the beginning of this journey with HLHS, wonder if our children (boys and girls) will be able to take part in athletics. Thank you for showing us that not only can they participate, but can really enjoy playing sports!
A Heartfelt Donation: The Mended Heart
How cute is this kimono? Adorable, right? And not to mention, so so practical for our heart babes - completely compatible with tubes, wires, and even the MRI machine!
Well, we’re excited to introduce you to one of our newest partners here at Sisters by Heart! Hospital gowns have long been a staple in our care packages (generously donated by EZ Axcess, Inc.), but when our demand far exceeded our supply, we knew we had to look to find an additional partner in this endeavor. We were beyond thrilled to happen upon Lara and her awesome shop, The Mended Heart. We had to order both girl...
and boy kimonos.
As soon as we received them, we were hooked! Lara has now partnered with Sisters by Heart to provide these adorable gowns at a deep discount, and we are SO grateful for both her talent and her generosity!
We asked Lara to share a little about how The Mended Heart was started…
“On September 1st, 2011, my youngest daughter, Mylah, was diagnosed with a CHD known as Tetralogy of Fallot. I was 34 weeks pregnant and shocked to hear the news. My husband and I learned all we could about her defect and prepared ourselves for life with a heart baby.
Born four weeks later, Mylah was healthy and very pink. She had her first OHS at five days old and it was a success. Mylah came home and gained weight and grew as she should.
At six months old on April 25th, 2012, she had her full heart repair. During that hospital stay she wore some adorable hospital gowns that her Grandmother made. Everyone commented and just couldn't get enough of them! That's when The Mended Heart really took off. I knew I needed to make more to share with other heart babies and families. I wanted to create awareness but also create something in Mylah's name. The Mended Heart has been a beautiful creative outlet for me and has helped me emotionally to deal with all I've had to after Mylah's diagnosis. It has grown and become a success for me. I am so excited to be partnered with Sisters by Heart and create awareness and help heart families!”
Thank you again, Lara, for partnering with us to bring adorable gowns to our families!
And, if you're as hooked as we were as soon as we saw them, you can check out more gowns and other CHD products at Lara's store, at The Mended Heart!
Fun in the Sun: Year Two
Last weekend, for the second year in a row, Sisters by Heart had its annual Board retreat in sunny Palm Springs, CA! We had an amazing weekend of bonding, brainstorming and planning for the year ahead. A super secret special project (that we can't wait to tell you about!).And lots (and lots and lots) of care package prepping. We'd like to extend a special thank-you to the Gerrish family for allowing us to use their beautiful home for the second year in a row. Thank you Gerrishes!
* Retreat soley funded by individuals, no donations or Sisters by Heart funds were used.