Practitioner’s Post: The Promise of Stem Cells
By: Sunjay Kaushal, M.D., Ph.D., Director of Pediatric Cardiac Surgery at the University of Maryland Medical Center
Dr. Sunjay Kaushal is a cardiothoracic surgeon with a passion for reconstructing the hearts of those battling critical congenital heart disease. During reconstruction, Dr. Kaushal also looks at the pediatric heart with an innovative eye. In talking to Dr. Kaushal, it’s clear that he’s dedicated not only to reconstructing the hearts of our babes, but also in finding ways to improve their lives for many years to come.
Thank you, Dr. Kaushal, for taking time out of your busy days to share your research and trials with Sisters by Heart and our families. There is so much hope in medical advancements and your continued work.
A few years ago, Dr. Kaushal began studying the positive outcomes with stem cell therapies, in the adult population, following damage to the heart after ischemic events (i.e. heart attacks.) He asked himself a simple question: If stem cells are assisting in the regenerative process for adults, can we use similar therapies for children? The short answer, he found, is yes.
Over the past year-plus, Dr. Kaushal preliminarily proved his theory – that infant heart tissue containing specific stem cells has the ability to: 1) survive outside of the body, 2) grow and multiply (yes, like Gremlins) and, 3) assist in recovery and strengthen heart function when injected into the heart. How did he prove this theory, you ask? He did it by testing harvested human heart tissue from 150 HLHS and CCHD patients and injecting them into animal models. Armed with quantitative information and data, he presented to the FDA for approval of a new clinical trial which is slated to begin soon at University of Maryland Medical Center.
Essentially, the clinical trial looks like this:
During the Norwood operation, heart tissue taken from the right atrium, which would routinely be discarded post cannulation, is instead banked for future use on that same patient. The harvested heart tissue is then grown to duplicate the patient’s own stem cells for reintroduction to the patient’s heart. Once expanded, the cells are placed back into the heart during the Glenn/hemi-Fontan operation via injection into the coronary arteries just prior to coming off bypass. The infusion of stem cells takes less than 4-5 minutes to complete.
The purpose of Dr. Kaushal’s trial is to determine how effective these specific stem cells are in regenerating heart tissue and strengthening the heart muscle/function in single ventricle patients. Obviously, a major risk factor with HLHS patients is heart failure. The theory is: inject the heart with its own, younger stem cells and the heart will regain a large percentage of function. So, is this possible? Dr. Kaushal believes so. He believes that based on the adult studies performed to date, the trial is both safe and effective. In the adult-based study, heart function improved by 12%. For those of you who are familiar with the term “ejection fraction,” the EF improved by 12%. That is a staggering improvement. Not only did the study show effectiveness, but it illustrated that the stem cells continued to work over a year’s time. At 4 months, the heart function/EF improved by 4%, at 8 months, 8% and over a year’s time an overall improvement of 12%. Dr. Kaushal cautions that we must remember that this is a Phase I study, which only examines safety issues. Resident stem cells will need to be evaluated for efficacy in a larger Phase II study that will be appropriately powered to eventually determine their efficacy.
Even more exciting… when Dr. Kaushal compared his preliminary results in children to that of an adult heart, he’s finding that the infant cell models outperform the adult models “3 to 1.” Therefore, the younger the stem cell, the more potent and effective it is in repair and regeneration.
Why does it work?
Researchers aren’t exactly sure. Dr. Kaushal will attempt to answer that question during his clinical trials with HLHS patients. The two thoughts include: 1) the new stem cells are secreting good proteins and therefore are improving function and/or 2) the new stem cells assist in preventing stress to the older cells. Either way, it’s promising news for parents of children with HLHS or any CCHD.
Imagine if surgeons and physicians can inject stem cells into the hearts of our children and dramatically improve heart function… We know we got the chills when thinking of the possibilities…
Dr. Kaushal’s trial is awaiting hospital approval. He’s also investigating the possibility of securing funding from both the public and private sectors so that parents can enroll their children free of charge.
How will we know if the clinical trial works?
Dr. Kaushal’s proposed clinical trial will enlist 30 HLHS patients and follow them over a year’s time, post-stem cell infusion at Stage 2 palliation. He will conduct a baseline MRI to measure function the morning of Stage 2. After Stage 2 and the injection/infusion of stem cells, he’ll perform repeat echocardiograms and MRIs at 6 and 12 months post-op to compare the heart’s performance and regeneration. No other tests are needed. Dr. Kaushal pointed out that the right heart (i.e. right ventricle) is “not normal” and very hard to assess on echo and therefore, the MRIs are needed to gain an accurate measurement.
Can my older HLHS child or HLHS adult benefit?
Yes. Plain and simple. Dr. Kaushal’s hope is that, once approved, his trial will illustrate and prove the theory that stem cell therapy is safe and effective for single ventricle infants and children. If that is the case, if a child or adult with HLHS, “down the road” experiences dysfunction, they can receive stem cell injections from banked/frozen cells. The frozen stem cells, after thawing for 2 months, are just as potent as they were before freezing.
What do we know now?
Data for stem cell therapy in infants and children living with HLHS is very scarce. Dr. Sano (who developed the Sano shunt for a modification to the Norwood) is conducting similar research in Japan but is using a different type of stem cell (still from heart tissue.) Dr. Sano is injecting cells into heart muscle at one month of age, shortly after the Norwoodprocedure.
Additionally, researchers in Germany have successfully used bone marrow cells in HLHS children. They’ve injected 10 CCHDers (not all HLHS) with autologous bone marrow stem cells and are seeing dramatic improvements in function. In fact, one child – an HLHSer in heart failure and listed for transplant – was injected with bone marrow cells while on the transplant list. The parents were willing to do anything to avoid transplant. And another lesson in asking many, many questions comes into play. They talked to doctors about their options and were told about the experimental bone marrow cell infusions. The parents agreed to the infusions and were ecstatic at its results. The child’s heart function improved significantly and subsequently, the child was removed from the transplant list. Based on his conversations with German researchers, Dr. Kaushal is gearing up for a similar study here in the United States using bone marrow cells for treating HLHS and dilated cardiomyopathy patients with depressed function.
What if I didn’t bank my child’s cord blood/tissue?
Don’t panic. The body is full of stem cells that can be harvested. Dr. Kaushal emphasized that there are no current treatments for HLHS, or any CCHDs, utilizing umbilical cord blood stem cells, although there are current studies ongoing at Duke University regarding the use of umbilical cord blood therapy for HLHS patients. Dr. Kaushal recommends, if you have the resources to bank cord blood/tissue, go ahead and bank. Medicine evolves and you never know what options will be on the table 5, 10, 15 years from now.
Dr. Kaushal and his team hold much enthusiasm and cautious optimism about their new clinical trial which, once approved to begin enrolling patients, could change the landscape of medical treatment for HLHS infants, children and even adults.
Trust us when we tell you, Dr. Kaushal, we’re ALL cheering you on and sending all the positive energy we can muster. Our children’s lives depend on it.
Watch Dr. Kaushal’s discussion on his clinical trial: http://www.umm.edu/media/video/kaushal-circ-study.htm
Sunjay Kaushal, M.D., Ph.D. is the Director of Pediatric Cardiac Surgery at the University of Maryland Medical Center. His special interests include pediatric CT surgery, neonatal heart surgery, fontan conversion, valve repair, adults with CHD and research with a focus on pediatric patients with HLHS and Cardiomyopathy. Learn more about Dr. Kaushal or contact him at: http://www.umm.edu/doctors/sunjay__kaushal.html#ixzz278rjvxNM
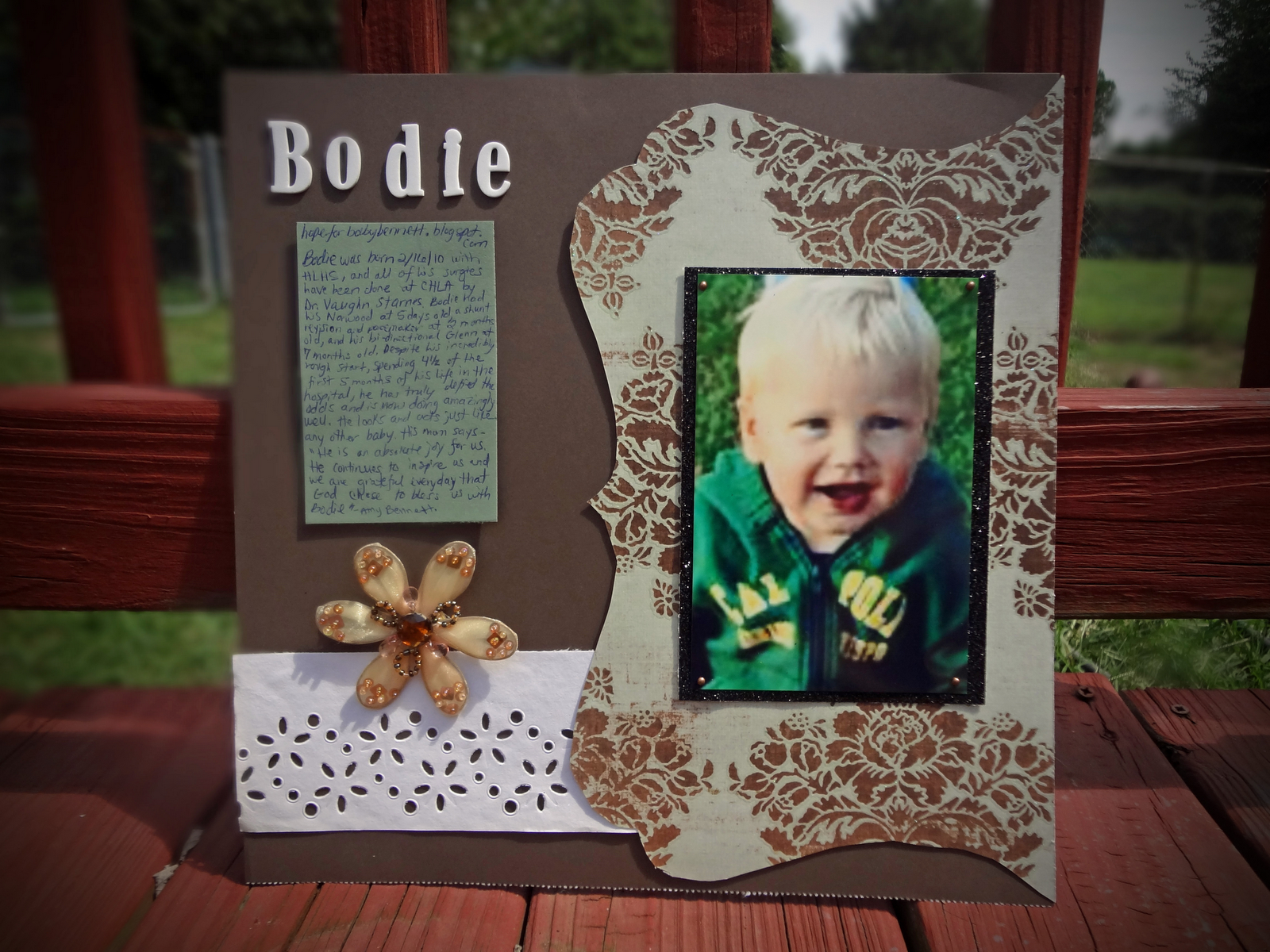
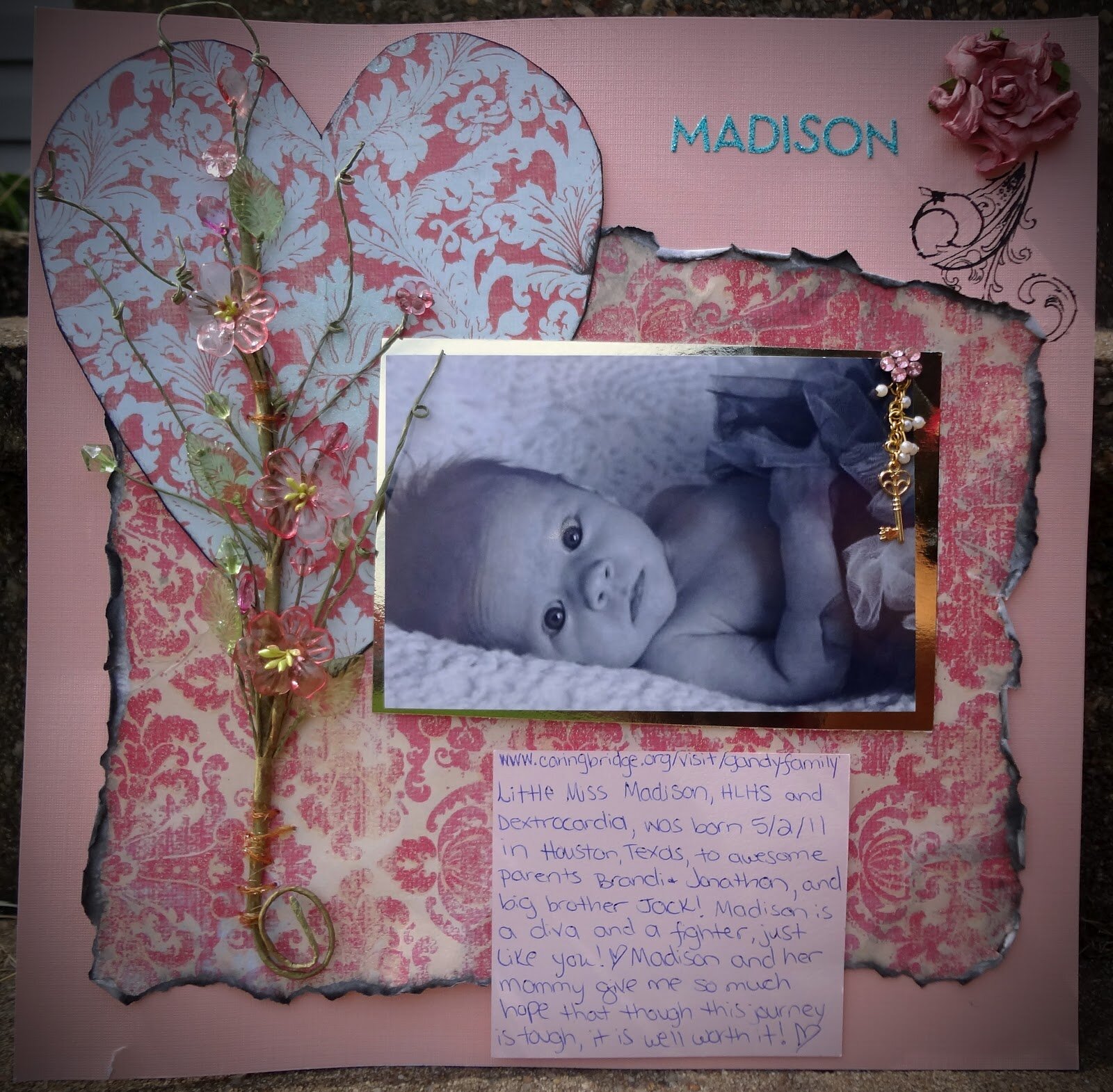
Creative Moms: Warrior Scrapbooking
A few weeks ago, we heard from one of our recipient moms, Sarah. Her daughter, Cecilia is inpatient and working diligiently on feeding in order to return home following her Norwood. Sadly, Sarah is not able to be at Cecilia's bedside 24/7 as her other children (5 adorable girls total) need her love and comfort as well.
To help ease some of Sarah's pain, she created a "Heart Friends" scrapbook for Cecilia - so she'd know she's never alone. It's true, Cecilia has many heart friends cheering her on. Sisters by Heart loved this idea and invited Sarah to share her creativity with you, along with some photos of Cecilia's book.
Getting Crafty with Sarah:
As a Heart Mom, we turn to each other for advice, support, and reassurance that we are not alone. We have places in our hearts reserved for each Warrior and Angel, and root for them just as hard as we do for our own child.
I wanted to make something for my HLHS fighter, Cecilia, to share stories of hope with her. And so, I came up with a scrapbooking project and included all of our "Heart Friends." As my intention began for Cecilia to find comfort in this scrapbook, it also served a purpose in bringing myself extra comfort. Creating Cecilia's Heart Friends book became a major coping tool for me, reminding me we are not alone, and as well reinforcing hope.
In this journey most of us will face depression or have trouble accepting that there is nothing we can do to fix our child's heart defect. Sometimes to keep us getting through the moment, it helps to focus on the Warriors who are thriving. It can be hard to watch your fighter with uncertainty, not able to let go and trust that they will progress and become another face of HOPE ♥. All of us need to focus, however we can, and stay positive. Heart Friends allowed me to stay focused and positive!
Whether you are crafty or not, and want to make a scrapbook, it can be a costly hobby. I often use non traditional embellishments, such as broken/unused jewelry, torn pages from old books, lace and trimming from old clothing, ect. You can find a large amount of tips here http://www.scrapbook.com/tips.php and I encourage you to browse through Layout Galleries for ideas and inspiration here http://www.scrapbook.com/gallery/?type=layout&f=1
Some of the pages I created for Cecilia's book follow - all HLHS warriors who've provided me with incredible amounts of HOPE.
I wish all of you the best of luck in your Journey. Cecilia and I will be rooting for you! ♥
~ Sarah, Mom to Cecilia (HLHS, 1 month old)
Thank you so much, Sarah, for sharing your creativity and incredible Heart Friends book with all of us. It's certainly something Cecilia will cherish for many years to come!
Remembering Our Heroes
As we approach the 11th anniversary of the attack on the World Trade Center, and honor the lives lost that day, we wanted to share a special story relayed to us; a story of a hero lost that day, and a very special HLHSer who lives on in his memory. Thank you Lauren for sharing your story!
Jack Foley at the Brooklyn Wall of Remembrance
"On September 11, 2001, my family was changed forever. My brother, FDNY FF Michael Kiefer, was one of the brave 343 firefighters who died a hero at The World Trade Center. Michael was only 25 years old when he was so violently taken from us. His life long dream was to be a FDNY Firefighter. After lots of hard work and determination, he graduated at the very top of his class. His dream was cut short after only nine months on the job when he answered his final call on September 11, 2001.
Ever since than our family has not been the same. Michael was the core of our family. He was an amazing big brother to my sister Kerri and I, and a loving son to our parents, Pat and Bud. Family was extremely important to Michael so when my sister and I were both expecting our first children together (we were due 11 weeks apart) it broke our hearts to know that our babies would grow up without their Uncle Michael.
When I first found out I was pregnant, I prayed to my brother everyday to watch over our baby. Michael's faith was very important to him. My 20 week sonogram was scheduled for the week after my brother's birthday. Being a believer in "signs," I took the timing of our sonogram as a sign that Michael would be with us. I remember sitting in the waiting room having a "not good" feeling. I reminded the technician numerous times that we did not want to know the sex of the baby. As the test went on I could tell that something was not right, the tech was very quiet. We were told that something was wrong with our baby's heart. I was so sure that they were wrong. After some other tests it was determined that our baby had Hypoplastic Left Heart Syndrome. I literally wanted to throw up when they told me exactly what it was and the prognosis for our child. From that moment on I think I spoke to my brother every second of every day and begged him to watch over his niece or nephew. The next few month were long and hard not knowing what would be.
Our son, Jack Michael, was born at Morgan Stanley Children's Hospital of Columbia Presbyterian on April 25, 2011. He was absolutely perfect! Looking at him you would never know he only had half a heart! Jack had his Norwood at four days old. I remember the morning of his surgery, my husband Rob and I came up from my room and we looked at Jack's monitor just like we always did when we came to his side. His heart rate read 132. I began to cry immediately! My brother was in Ladder Company 132 on 9/11! As I walked the hallway to Jack's side that morning I begged Michael to be with him during surgery. I got my sign with his heart rate reading! It had never read that before that I had noticed so to me that was Michael letting me know he was with Jack! Surgery went amazing and he recovered quickly and we were home a week and a half after surgery! Jack had his Glenn at 4 1/2 months old and once again he did amazing! We were home four days after surgery.
Thankfully, Jack continues to defy the odds and is doing well! I have no doubt that Michael is with Jack every step of his journey. I like to believe that Jack and Michael had a little talk up in Heaven before he came to us. Michael let him know that he was going to have to be strong and I believe he gave Jack a lot of his strength! Just the other night my mom innocently asked Jack "where do you get your strength from?" He immediately pointed to my brother's picture! It was the first time anyone asked him that question and with his response tears ran down my face! Jack and my nephew, Michael Anthony, know their uncle so well and it makes us all so happy! The picture above was taken at The Brooklyn Wall of Remembrance in Coney Island, NY. We took Jack there and he found his Uncle Michael's picture and lovingly pointed to it and then blew him a kiss. Michael may not be here physically on earth but his memory will live on forever. His nephews will grow up knowing how much their uncle loves them. Jack's journey is a very scary and long one but I know he has the very best Guardian Angel watching over him! Please never forget the sacrifices made on September 11, 2001!"
~Lauren Keifer, mom to HLHSer Jack Michael Kiefer
Thank you again Lauren, for sharing this heartwarming picture of Jack and the story of your brother; two amazing, inspiring heroes.
Top Ten (or 14) Discharge List
This past week, via our Facebook page, we requested feedback from HLHS families to assist us in preparing a Top Ten Discharge List we feel is necessary following birth and the Norwood operation. We received great feedback from moms and dads across the nation.
The information received was compiled into the following list, shared this past weekend at the JCCHD's Semi-Annual National Pediatric Cardiology - Quality Improvement Collaborative Conference. The Conference attendants included pediatric cardiac teams from across the country. The teams thoroughly appreciated our insights and loved the Top Ten List, which turned out to be "Top Ten" - plus a few necessary extras which we couldn't allow to go by the wayside.
Since so many of you provided input, we wanted to share the finalized list with you. Feel free, particularly new families and those soon-to-be-discharged, to print out the following list and go over it with your health care team.
Discharge: The Top Ten Things You Can Do to Best Prepare a Parent for Interstage
1. All parents should be armed with an interstage monitoring program and the necessary supplies for interstage care and monitoring: Pulse ox machine, infant scale, care binder or dedicated pages to record specific information (BP/Sats/Weight/intake, meds given, etc.). Most interstage parents feel that all of these supplies are necessary tools that help parents track changes and concerns during the interstage period. “Interstage monitoring” training should begin in the step-down unit so parents can get the hang of it for a few days prior to discharge.
2. Provide the parent a medication chart with dosage/administration directions, a proposed medication schedule and medication precautions list. The provided chart and schedule helps to eliminate parental anxiety regarding medication administration. Be certain parents know where they can obtain compounded medications before leaving the hospital. If the hospital pharmacy can provide a supply of oral syringes and caps, parents would be very appreciative.
3. Provide a nutrition and feeding schedule and contact information for a nutritionist/dietician when questions regarding feeding arise. Feeding issues occur over and over for interstage parents and we feel that a dedicated nutritionist/provider would greatly benefit our infants.
4. Recommended guidelines regarding exposure to outside risks (hand washing, sanitizing, visitors, etc.)
5. One-page handout delineating signs/symptoms of known complications along with contact information for a cardiologist or cardiac nurse practitioner which may be used at any time (24/7) for emergent situations. Additionally, provide an email address for this same provider for non-urgent questions and concerns. Parents feel like they are on a deserted island once home with their fragile HLHSer. Knowing that you have a trained professional to contact 24/7 is a must for interstage parents.
6. Infant CPR education and training along with infant CPR instructions to post on the refrigerator at home.
7. Handouts regarding sternal care, scar and infant massage and physical therapy that can be done in-home by the parent during the interstage period. These modalities provide a way in which parents feel they can take control over their uncontrollable situation. Giving parents something they can “do” to help their infant is a simple and easy gift that cardiac centers can give a parent.
8. Talk to your parents! Be certain they realize what being an interstage parent means – they will essentially be a nurse/doctor without a degree during those interstage months. Interstage is very much an isolating 4-plus months, which is “normal” for interstage families. There are tools provided by non-profits to find other interstage families. Encourage your families to check out Linked by Heart (www.linked-by-heart.org). Encourage them to reach out to others in similar situations to help ease the burden, gain a sense of community and diminish the sense of isolation.
9. Advise parents about REFLUX and that it is extremely common. What are the signs of reflux? Can dosages be increased? Can you order a change in reflux medications if one reflux med is not effective after a month or two? Provide tips on how to counteract reflux or avoid flare-ups.
10. Allow parents to TRUST THEIR OWN INSTINCTS. No question or concern is too small at this critical time. We’ve been given the task to keep an extremely fragile infant alive for several months and we want to be empowered with our “gut instincts.” Many times, the parent’s gut is accurate and we want to know you are listening to our thoughts and concerns.
Other areas of importance to an interstage parent:
11. Is there a communication plan between the treating cardiologist and pediatrician?
12. Social work can play a larger role in most centers to help parents prepare for interstage. Is insurance coordinated with supply companies, are parents set up with a compounding pharmacy, are there programs (WIC, Medicaid, Early Intervention) that can be applied for/set up prior to discharge, etc.? All of these things are horribly burdensome for a parent to figure out while they’re extremely anxious and doing all they can to keep their child alive.
13. Advise parents not to compare their child to another HLHS infant. All of these children come with their own complications and set of circumstances. This is often easier said than done, but a reminder prior to discharge is extremely helpful, especially when coming from a medical professional.
14. A pre-discharge meeting with child’s surgeon or cardiologist to explain the Norwood/hybrid, draw diagrams of their child’s heart post-op and explain what took place during surgery. Often, we are in such shock pre-operatively that we only retain half of what is stated. Each parent should have a good understanding of their child’s cardiac anatomy and their child’s baseline saturations and heart rate. This is particularly helpful if the infant was not prenatally diagnosed.
An additional item currently being developed by the Collaborative (which we all think is great), is the Patient Information Instruction Card. This card, or something bearing similar information, can be kept in your purse or wallet in case of emergencies. It's a simple tool that allows emergency providers the pertinent information they may need to assess your HLHS interstage infant (i.e. your child's typical blood pressure, saturations, known complications and medications).
Thanks again to those who contributed to this Top Ten List and who continue to support Sisters by Heart and work with us to improve the landscape for HLHS infants and children.
Practitioner's Post: Stem Cell Research for the HLHS Patient
If you've been following us on Facebook or Twitter, you've likely seen our posts and tweets about Dr. Timothy Nelson and the HLHS Research Program at the Mayo Clinic in Rochester, MN. The information Dr. Nelson and his researchers shared with Sisters by Heart is extremely fascinating and provides great hope (and a serious sense of urgency) for all of us affected by Hypoplastic Left Heart Syndrome. Thank you Dr. Nelson and the program's research coordinator, Julia, for sharing the latest developments in regenerative medicine for the HLHS patient.
By: Timothy Nelson, MD, PhD, program director of the Todd and Karen Wanek Family Program for Hypoplastic Left Heart Syndrome at Mayo Clinic
I’m Timothy Nelson, MD, PhD, program director of the Todd and Karen Wanek Family Program for Hypoplastic Left Heart Syndrome at Mayo Clinic. The goal of our research program is to develop innovative clinical trials that offer the latest advances in cell-based therapy that could be used to treat people with HLHS.
Upon completing the three stages of surgery, HLHS is ultimately a disease of the right ventricle that becomes too weak to be able to sustain normal cardiac function. Fortunately, surgical procedures over the last two decades have lead to dramatic improvement in the care of children with HLHS, but many questions remain unanswered.
Through our research, we hope to better understand the causes of HLHS, to develop a system for predicting right ventricle performance, and to determine whether or not the patient’s own stem cells could potentially be an effective treatment. Understanding whether stem cells are dysfunctional in patients with HLHS or whether they are normal will be very important to help determine whether the use of stem cells or regenerative medicine could be an appropriate therapeutic strategy. Who is the right person for regenerative therapies? What are the right types of stem cells? When is the right time for this potential therapy? To answer these questions, we are focusing on research studies that involve families affected by HLHS.
Our program is focused on the next generation of therapies that could be used to improve the function and long-term performance of the right ventricle – one of the potential therapies being regenerative medicine through the use of stem cells. Regenerative medicine is the process of regenerating human tissues with new building blocks to heal or replace damaged or diseased tissue. This would be similar to planting a seed in order to grow a flower. Stem cell therapies aim to transplant “stem cells” into damaged hearts with the goal of growing new heart muscle.
Bioengineered stem cells start with the collection of tissue, such as discarded skin from a surgical procedure, and are then converted into stem cells that can acquire a new ability to grow into heart muscle. These stem cells – and ultimately the bioengineered heart muscle derived from these cells – originate from the patient’s own body. These cells can then be studied in the laboratory to further understand the molecular causes of HLHS, and hopefully provide a powerful tool to better customize innovative solutions for people with HLHS.
To see video regarding the bioengineering of stem cells, watch this fascinating video; the video depicts how Dr. Nelson is creating bioengineered tissue for HLHS research.
Dr. Nelson's team shared with us the video clip of the beating cardiac tissue he's created in the lab.
Regenerative medicine strategies and stem cell-based therapeutics have been applied to heart disease in adult patients over the last 8 years. This experience allows us to consider the possibility of applying similar technology to patients with HLHS and other congenital heart disease. Although this is not yet available, the promising vision of this regenerative approach becoming a reality requires significant scientific and preclinical research studies to be the focus of today. We are fully dependent on the participation of families affected by HLHS in order to generate the data that is required to make the new discoveries and innovations for the clinical practice of tomorrow.
Although we don't yet know that stem cells will be used in the care of patients with HLHS, this type of research will be paramount for the scientific community to be able to make an informed decision as to the safety and efficacy of such hopeful therapeutic strategies. Ultimately, we hope our research will result in the ability to delay, or prevent, the need for heart transplants in people with this congenital heart condition. More information about the ongoing research for HLHS can be found at:
http://mayoresearch.mayo.edu/mayo/research/hypoplastic-left-heart-syndrome/
If you have specific questions regarding Dr. Nelson and his team's research, feel free to contact them at: hlhs@mayo.edu
The Practitioner's Perspective: Dental Care and Congenital Heart Defects
By: Michelle M. Kelman, DDS
Pediatric Dentist, Cedars-Sinai Medical Center, Department of Surgery, Dentistry, UCLA School of Dentistry, Pediatrics
“Go brush your teeth.”
It’s a phrase that most children feel they hear too often. There is so much to do at the start and then the end of the day that all too often, tooth brushing is overlooked. Studies have shown that children with congenital cardiac disease (CCD) have poor oral health compared with healthy children. As you may already know, children with congenital heart disease (CHD) are at risk for bacterial endocarditis, an infection of the tissue that lines the heart and blood vessels. It is important for your child’s health to keep the oral cavity healthy to prevent infection that may begin in the mouth.
Some important facts to consider:
Studies have shown that children with CCD suffer poor oral health, compared with heart healthy children. This is most likely related to a combination of abnormal dental formation associated with the cardiac condition and dental neglect.
Children with CCD are more likely to have abnormal tooth formation including developmental enamel defects such as weakness in enamel, are more prone to malocclusion that includes crowding of teeth, and are more prone to harmful gum disease, compared with heart healthy children.
The chronic intake of sweetened medications is associated with increased cavities in children with CCD.
Children with CHD are prone to develop infective endocarditis from bacteremia not only induced by dental procedures but also from chronic poor oral health. Untreated dental decay may develop quickly into pulp infections which are associated with bacteremia, endocarditis, and even brain abscesses in children with CCD.
In regards to dental treatment, severely affected children may have reduced tolerance to the stress induced by dental treatment. Complications of CCD such as hematological, respiratory and immunological problems, and drug interaction with chronic medications must all be considered for children with CCD.
Unfortunately, a significant number of children with CCD do not receive optimal professional dental care until the child already has a mouth full of cavities. The goal is to prevent this. Here are some oral health guidelines to follow:
Home Oral Care:
Start taking care of your children’s gums before the first tooth erupts. Wipe down the gums after every meal, especially after medications.
Help your children with their toothbrushing. Children under the age of eight do not have the manual dexterity skills to brush on their own.
Teeth should be brushed for two minutes at least twice a day. As most medications are very sugary, it is recommended that your child brushes after medication is given.
Flossing: Children’s Flossers are recommended because of their ease of use. Because of tooth crowding, food/ sugary medications get stuck in between the teeth. It’s essential to floss the teeth to get the food out from in between them and from the gum line.
Tooth Wipes: It is recommended that you carry tooth wipes with you for “on the go” situations. It is recommended to wipe your child’s teeth following medication.
Diet: Avoid excessive sugar intake and “sticky” foods such as hard candies & even food that you feel is "healthy" like raisins (still "sticky"!) As soothing as sticky candy may be, a scoop of sorbet is much better for the teeth than a jolly rancher.
Seek out a knowledgeable dentist:
Your child should be seen by a pediatric dentist by the age of one. Make sure the dentist you have chosen has experience treating children with CCD. Please arrange for your cardiologist to send over a complete medical history and recommendations for treatment prior to your child’s first visit. Most children with CCD do not need premedication with antibiotics. The pediatric dentist and your cardiologist are familiar with the latest guidelines and will determine if premedication is needed.
Your pediatric dentist will form a preventative treatment plan that may include more frequent cleanings.
Your dentist may prescribe topical fluoride therapy and fluoride supplementation.
As the molars develop in the mouth, your pediatric dentist may recommend sealant placement on all molars with deep grooves and fissures. This will help prevent the entrapment of food/ sugar in these grooves and thus assist in preventing the formation of cavities.
If your child already has cavities that need to be filled, your pediatric dentist will coordinate with your cardiologist a treatment plan that will place the least amount of stress on your child. This may include treatment under General Anesthesia with an anesthesiologist that specializes in high risk pediatric patients.
To conclude, the time to start taking care of your child’s teeth is before the first tooth erupts. Brushing and flossing properly at home, and having regular dental visits, from a very early age, is essential.
Michelle M. Kelman, DDS
Pediatric Dentist
Cedars-Sinai Medical Center
Department of Surgery, Dentistry
UCLA School of Dentistry, Pediatrics
For more information on the American Heart Association guidelines for antibiotics prior to dental care:
http://www.ada.org/2157.aspx#heart
http://www.ada.org/sections/professionalResources/pdfs/patient_75.pdf
A special note from Sisters by Heart:
In addition to February being Congenital Heart Defect Awareness Month, it is National Children's Dental Health Month. All information here is for the purpose of helping you care for your child with a Congenital Heart Defect (and your healthy heart children, too!) However, please consult with your dentist regarding personalized care and a treatment plan for your child. This is very good general advice, but does not take the place of seeing a dentist. If you are not currently implementing these practices in your child's oral hygiene, it is a great time to start. No need to panic if you have some room for improvement in your home care and also if you have not had your child see a dentist yet. You may get recommendations/referrals from your cardiologist, pediatrician, and/or your adult/general dentist. No matter the age of your child, it's a great time to seek out a dentist who can work well with your child, your cardiologist, and you! ~Sara Hale, Sisters by Heart Mom/DDS
The Practitioner's Perspective: The Genetic Link
By: Paul Grossfeld, M.D., Associate Clinical Professor at UCSD School of Medicine and Attending Pediatric Cardiologist at Rady Children’s Hospital in San Diego
We’re excited to bring you the following post from Paul Grossfeld, M.D., Associate Clinical Professor at UCSD School of Medicine and Attending Pediatric Cardiologist at Rady Children’s Hospital in San Diego. Dr. Grossfeld spent many hours caring for one of our own Sisters by Heart warriors, Travis DiCarlo, and subsequently spent time discussing his research with Travis’ parents, Roger and Nicole. Dr. Grossfeld’s research lab is working towards identifying the specific genetic causes of congenital heart defects in order to improve therapies and ultimately lead to prevention. Dr. Grossfeld’s lab is 50% funded by the Children’s Heart Foundation with the remaining funds coming from private fundraising efforts. It is our hope that funding for promising research, such as Dr. Grossfeld’s, improves drastically to increase awareness for CHD and the countless lives they effect.
Thank you so much Dr. Grossfeld for sharing your research with us!
Congenital heart defects are the most common type of birth defect, affecting almost 1% of all newborn infants. Hypoplastic left heart syndrome (HLHS) accounts for a small percentage of all heart defects, but remains one of the most common causes of death in infants with congenital heart disease. Although most cases of HLHS and other heart defects are due to a genetic cause, a specific disease-causing gene mutation is only known in about 10% of patients. Clearly, identifying the specific genetic causes of congenital heart defects will improve therapies and ultimately lead to prevention.
We have embarked on a multidisciplinary approach involving human genetics and genetically engineered animal models to identify genes for congenital heart defects, including HLHS. The first approach has focused on a rare chromosomal disorder called Jacobsen syndrome (11q-), caused by deletions in the 11th human chromosome. These patients have the highest frequency of HLHS of any known human genetic disorder, as well as many of the most common congenital heart defects that occur in the general population. The second approach entails studying other chromosomal disorders associated with congenital heart disease. Specifically, with recent technological advances, patients with congenital heart defects can be analyzed to identify microscopic losses or gains of chromosomal material that contain genes that cause congenital heart defects.
We have recently identified several new chromosomal disorders that likely harbor previously unidentified disease-causing genes for congenital heart defects. Lastly, with the amazing advances in DNA sequencing technologies, it is now feasible to perform direct DNA sequencing on the entire genome (i.e., of all ~30,000 genes) to identify a putative disease-causing mutation. Taken together, these three approaches are enabling us to identify numerous new “candidate disease-causing genes.”
Due to obvious limitations in human genetic studies, we have utilized genetically engineered animal models to study the function of candidate genes in heart development, and to establish causality for specific heart defects. Towards that end, we have demonstrated that deletion of a single gene in the mouse that is deleted in Jacobsen syndrome causes heart defects, including a hypoplastic left ventricle and ventricular septal defects. We are also using simpler organisms including zebrafish and chicks to understand further the functions of these genes. These studies allow us to identify the specific cellular lineages in cardiac development, which could lead to new strategies for the prevention of congenital heart defects.
We are also embarking on a recently developed technology that allows human skin cells to be “reprogrammed” into developing heart cells. As described above, specific lineages in which the causative gene is known to function can then be studied to characterize the mechanism by which absence of the gene causes heart defects, so-called “disease in a dish”. This extraordinary technology will eventually lead to the identification of putative drugs that could potentially preserve the function of these cellular lineages during heart development, thereby preventing some types of congenital heart defects.
Click here for a list of Dr. Grossfeld’s publications.
To support Dr. Grossfeld’s research, please mail checks to:
UC San Diego
Health Sciences Development
200 West Arbor Dr. #8982
San Diego, CA 92103-8982
Attention: Shawna Fallon
Payment can be made to: “UC Regents #42364”
To make a donation over the phone, please call 619-543-3499.
94% of all donations go DIRECTLY to support Dr. Grossfeld’s research!!!
Practitioner's Post: Grief and HLHS
By: Dr. Kenneth J. Doka, Professor and a Senior Consultant to the Hospice Foundation of America
All of us at Sisters by Heart experienced a significant sense of loss at the time of our child's diagnosis of Hypoplastic Left Heart Syndrome, and continue to grieve throughout our journeys with HLHS. While we don't always identify our feelings as grief, that is what we experience.
Grief: deep and poignant distress caused by or as if by bereavement; also: a cause of such suffering
To help identify some of the feelings associated with grief, this chart identifies the journey from "'normal' functioning" to the "return to meaningful life."
With grief playing such a large role in all HLHS journeys, we reached out to one of the nation's leading experts on grief, Dr. Kenneth J. Doka. Dr. Doka is a Professor and a Senior Consultant to the Hospice Foundation of America. He's written countless books and articles on grief and offering new perspectives on grieving.
Dr. Doka, extremely touched by our HLHS community and all that we endure, took the time to explain what happens once we, as parents, receive a diagnosis of HLHS for our infants.
Thank you, Dr. Doka, for providing the following Practioner's Post regarding anticipatory mourning.
Kenneth Doka, Ph.D.
Anticipatory Mourning
Feelings of grief that develop before, rather than after, a loss.
If we have ever heard of anticipatory grief or anticipatory mourning, we are likely to think of it as the grief that we experience when we expect or anticipate a loss such as the death of our child. In truth, the concept is much broader than that. One of my colleagues, Dr. Therese A. Rando, the author of a book on anticipatory mourning once called the term a “useful misnomer.” What Dr. Rando meant is that grieving an anticipated death is only part of what the concept means. As she redefines it, the term actually refers to all the losses that we experience as part of an illness whether or not the illness is, in fact, fatal.
These losses can be extensive in HLHS. It begins with the identification of the defect. We never expect our child to be born with a life-threatening illness. From the very moment of diagnosis, our world is turned upside down as our new born baby begins a seemingly never-ending series of surgeries. We mourn the loss of normalcy – the expectation of the child’s milestones here becomes fears for survivorship.
We may experience other losses as well. While rates are declining, many children born with HLHS experience developmental delays, neurological difficulties, learning disabilities, and chronic health problems. As the child ages and becomes aware of their condition, they too may grieve the condition.
All of these are losses too that need to be grieved.
This grief is a normal and natural response to the losses that parents, grandparents, siblings – all who love the child – will experience. It is natural too that the older child will grieve this condition as well.
Acknowledging the legitimacy of that grief is an important first step. We need not look at our grief as a betrayal or lack of hope. It is simply a response to loss. Once we acknowledge our grief, we can examine how we are coping with our losses. Gaining information, getting support, and joining with other parents are often helpful steps as we face a reality we never expected to or should have to face.
Kenneth J. Doka, PhD
Professor, The Graduate School, The College of New Rochelle
Senior Consultant, the Hospice Foundation of America
For additional information on Dr. Doka's work, please visit his site and publications list at http://www.drkendoka.com/.
We, at Sisters by Heart, want you to know that grieving is an ever-evolving process. Some days are certainly better than others. Just as Dr. Doka suggests, Sisters by Heart is here to help you: gain information, find support and connect with others to help make this journey a bit less strenuous. You are not alone in this journey!
For additional information on Dr. Doka's work, please visit his site and publications list at http://www.drkendoka.com/.
We, at Sisters by Heart, want you to know that grieving is an ever-evolving process. Some days are certainly better than others. Just as Dr. Doka suggests, Sisters by Heart is here to help you: gain information, find support and connect with others to help make this journey a bit less strenuous. You are not alone in this journey!
The Practitioner's Perspective: How to Choose a Congenital Heart Center
We're so excited to start a new series of guest blog postings from various practitioners who deal with our special kids on a regular basis. First up is Anthony Rossi, MD, the Director of the Cardiac Intensive Care Program at Miami Children's Hospital! He provides a unique perspective on how to go about choosing the right Congenital Heart Center for your child. Thank you so much Dr. Rossi for providing our inaugural practitioner's post!
By: Anthony Rossi, MD, Director of the Cardiac Intensive Care Program at Miami Children's Hospital
First, I am a practicing pediatric cardiologist at Miami Children’s Hospital. I am currently directing the cardiac intensive care program here. I’ve directed a cardiac intensive care program since 1989. I suspect I have directed a cardiac intensive care program longer than just about anyone who’s currently doing it. At best, I can speak from experience. At worse, it just makes me old! What I say is my opinion and my opinion only. However, what I will suggest to all of you is what I would suggest to any family member that might be in the same position as you. There might be some physicians out there that disagree, Or more likely, I’ll say things that they believe but won’t say publicly. So just think of me as your personal, inside source. Feel free to email me if you have a question at Anthony.rossi@mch.com. I’m more than willing to tell you who I think is the best at what we do.
If you are reading this, you are unlucky enough to be the parent of a child born or soon to be born with congenital heart disease. Or you just might have someone close to you in that unfortunate position. Here’s my message, don’t despair, don’t give up, it can and usually does get much better. And you have the potential to really influence the outcome in a positive way.
It was probably just a short time ago when you felt that you didn’t have a care in the world, and everything in life was as great as it could ever be. Perhaps you were pregnant, with marvelous expectations of the new life you were about to deliver to the world. A child who would be strong and smart and kind. A child who would go on to do great things.
The devastating news that your child has congenital heart disease can come in many ways. Perhaps your child had already been born and was apparently well in the newborn nursery. Occasionally your baby has been whisked away to some other hospital before you had a chance to kiss him/her goodbye. Sometimes it’s just a routine trip to the pediatrician for a “well-baby visit”. And then your whole world came tumbling down. Congenital heart disease can present in a number of ways, none of them are anything but horrific for a family. Even lesions that your cardiologist insists aren’t a big problem to fix mean years of unplanned visits to the office at best and “simple” heart surgery at worse. Simple heart surgery? It’s catastrophic to learn that any child needs to have any type of heart surgery, and there’s nothing simple about any of this, at least to a parent.
When I was in college (a Jesuit school at that) I learned the definition of despair was to be put in a position where you feel like you have no influence on the outcome. I am certain that this is exactly how every parent feels after learning their child was born with heart disease. I mean we were all taught, count the toes, count the fingers, all there so all good, right? Wrong! Who told us we needed to count the heart chambers?
But today, the news for children with congenital heart disease is better than it has ever been and the advances are occurring at a breath taking pace. The unfortunate part of this is that it’s often up to the parents to make sure that their child is getting the very best and most up to date care. Today, there are about 120 centers in the United States that perform congenital heart surgery and most will do it very, very well. In 1988, I was lucky enough to be in Philadelphia and if you had a child with HLHS, it was about the only place in the world where surgery for that problem was even offered. Babies came from around the world in hopes of saving their lives. In 2011, there are dozens of centers in the United States who have results that are now superior to the results we had in Philadelphia by Dr. Norwood himself. That’s amazing news. Back then, we could not be sure that the majority of these children who survived their surgeries would not grow up and become “cardiac cripples.” Every time a child comes back years after his/her surgery and looks great we take it for granted they are supposed to look like that. Twenty years ago we had no idea. As cardiologists all we could do was hope. We’ve now learned that these babies can grow up and lead very productive lives. They are in every way the blessing we believed they would be.
So when you’ve learned your child has congenital heart disease, what do you do? First, take a deep breath. Get the details. Listen. The more information you have, the better the chance you’ll make an informed decision. I will make a sports analogy here; major league baseball teams all have amazing athletes. They are the best of the best in the world. But all major league teams are not the same. It’s just human nature, we are all not created equally and some of us are better than others. Yes, weak teams will win games occasionally, but not as often as The Yankees, Red Sox or Phillies. Not all heart centers are created equally either. If you want to increase your odds of winning, go with the best.
When your baby is born with congenital heart disease
Sometimes things seem quite emergent and decisions need to be made rapidly. In actuality, there aren’t many problems (even serious ones like HLHS) where you don’t have the opportunity to take your time to do your homework and make the right decision. Usually most babies with heart disease are stable if medicines like prostaglandin E1 are used. There are some rare occasions where cardiologists need to act fast, but this is only in a minority of cases.
OK, first question to your doctors, how many of these cases do you see, and how many of these procedures have they done here? How many of these procedures has this particular cardiologist or surgeon done themselves? What are the outcomes for your doctor in this program for this problem? Don’t let them skirt the issue. Demand answers. Even in the very best centers, there will be the physicians with less experience, like those out of training. If you want to increase your baby’s odds, you need to ask these questions. Are there people here with more experience? Are there centers with more experience? Some metropolitan areas may have a number of congenital heart centers. They are NOT all created equally. You can be at a great medical center, but congenital heart surgery may be one of their weaker specialties. A great center might be down the street or perhaps an hour away. You won’t know unless you ask. I worked in New York City for almost a decade; there were about 7 centers performing congenital heart surgery. You could have, by chance, ended up in any one of these. But I can tell you that your child’s likelihood of having a successful outcome was greatly enhanced if you were in one of the top 3.
If you have no other data available, then the total volume of congenital heart surgery for a center and for a surgeon, and the number of these particular types of cases they have done, are probably the best indicators of excellence you can have. If you don’t have time for more extensive research, most of the time the volume data will lead you in the right direction. In all human endeavors, human factors play a huge role in surgical success - experience counts. Are there a number of surgeries a center needs to do to be great? Some reports suggest 300 cases per year. The Society of Thoracic Surgery considers programs that perform 200 open heart cases a year to be large. In general you want to be there, especially if the problem is either rare or complex. So ask, is this the largest program in the region? Now there are some great congenital heart surgical centers that perform smaller number surgeries than the numbers I’ve presented. I just personally believe the odds favor the bigger ones. One final thought, I suppose you can be too large. McDonald's makes the most burgers in the world, but probably not the best. Be sure you don’t feel like you’re in a factory or your baby is just a number (or your child is not just a referred to as a disease-“the hypoplast in bed two”).
Ok, so we established that experience counts (that coming from an old guy)! What else matters? The overall quality of the hospital or medical center is important. You want to know that everything matters in that center. From the quality of the surgeon to the center’s obsession with cleanliness. Ok, quick check. Look at the floors. Are they as clean as you like? If not, I suspect that hospital is slacking in other areas as well. Great hospitals are sparkling clean. I promise. A great center will have great sub-specialty doctors. Great centers have leaders in their field. If you Google your doctors, do scholarly articles come up? Not all great medical centers have great congenital heart programs, but it is impossible to have a great congenital heart program in any center that isn’t great.
How about the congenital heart program. Do they have all the pieces? All programs will have echo, but do they have dedicated echo physicians who have trained in noninvasive imaging? How about cardiac catheterization? How about electrophysiology or MRI? Do they have a dedicated cardiac ICU program? Will your child be cared for by physicians and nurses who care for asthmatics and diabetics and patients with pneumonia or will he/she be cared for by specialists in cardiac ICU?
Of course, so much of this comes down to who your surgeon is. I guess it’s the single most important factor. How do you know he’s the right one? Experience counts, what are his numbers? How many years has he done these operations? Where did he train? Was it one of the best congenital heart centers (say top 20 US News and World Report)? Most importantly, when you meet him, do you trust him? Does he look you in the eye? Does he have time for you? Is he annoyed when you ask questions? Is he annoyed if you ask for a second opinion (all great physicians are never put off by asking for a second opinion-it’s a big red flag if they are, they probably lack confidence).
OK, after 20 years of this, I could go on for ever. So I’ll summarize.
Do your homework. There are great sites available that should help steer you in the right direction. Two of these include:
http://health.usnews.com/best-hospitals/pediatric-rankings/cardiology-and-heart-surgery
http://www.youtube.com/user/Redmond111
But don’t believe everything you read on the internet. There’s nothing that prevents people from stretching the truth a bit on the internet.
Ask questions. Lots. If the explanation doesn’t make sense ask again. If you still don’t understand, it’s not you, it’s the person explaining it to you. Red flag!
If you have no other data, go to a center with more experience, one that does more surgery. Ask if there is one close or a center of excellence for your baby’s particular problem in the US.
Make sure you are in a comprehensive congenital heart center that has all the specialties covered, and make sure they have more that one of each (what happens if you need a cath and the cath guy is on vacation)?
Dedicated cardiac ICU, dedicated cath lab. Insist.
Know that you have all the rights. It is your child, not the hospital’s. You can advocate getting your child transferred to another center if you wish.
So that’s it for now. Good luck to all of you. You’re already on the right track. That’s how you found this web page. Continue to follow your instincts; they will lead you in the right direction. Oh yeah, ASK A LOT OF QUESTIONS.
Anthony Rossi, MD
Director, Cardiac Intensive Care Program
Miami Children's Hospital